- Record: found
- Abstract: found
- Article: not found
Venovenous Extracorporeal Membrane Oxygenation in Intractable Pulmonary Insufficiency: Practical Issues and Future Directions
Abstract
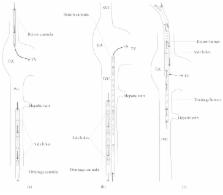
Venovenous extracorporeal membrane oxygenation (vv-ECMO) is a highly invasive method for organ support that is gaining in popularity due to recent technical advances and its successful application in the recent H1N1 epidemic. Although running a vv-ECMO program is potentially feasible for many hospitals, there are many theoretical concepts and practical issues that merit attention and require expertise. In this review, we focus on indications for vv-ECMO, components of the circuit, and management of patients on vv-ECMO. Concepts regarding oxygenation and decarboxylation and how they can be influenced are discussed. Day-to-day management, weaning, and most frequent complications are covered in light of the recent literature.
Related collections
Most cited references111
- Record: found
- Abstract: found
- Article: not found
Extracorporeal Membrane Oxygenation for 2009 Influenza A(H1N1) Acute Respiratory Distress Syndrome.
- Record: found
- Abstract: not found
- Article: not found
An expanded definition of the adult respiratory distress syndrome.
- Record: found
- Abstract: found
- Article: not found
Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score.
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.