- Record: found
- Abstract: found
- Article: found
Heart rate, intelligence in adolescence, and Parkinson’s disease later in life
Read this article at
Abstract
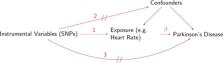
To investigate whether physical and cognitive fitness measured in late adolescence was associated with future risk of Parkinson’s disease (PD). The cohort included 1,259,485 Swedish men with physical fitness, body mass index (BMI), resting heart rate (RHR), blood pressure, intelligence quotient (IQ), and stress resilience measured at the age of 17–20 in relation to conscription. Incident cases of PD were ascertained from the Swedish Patient Register. Hazard ratios were estimated from Cox models, after controlling for multiple confounders. We further performed Mendelian randomization (MR) analyses to assess the causality of the associations, using GWAS summary statistics with > 800,000 individuals. During follow-up, we identified 1,034 cases of PD (mean age at diagnosis = 53). Men with an RHR > 100 beats per minute had a higher risk of PD compared to men with an RHR of 60–100 beats per minute (HR = 1.47; 95% CI = 1.08–1.99). Men with IQ above the highest tertile had a higher risk of PD compared to men with an IQ below the lowest tertile (HR = 1.46; 95% CI = 1.19–1.79). We found no association for physical fitness, BMI, blood pressure, or stress resilience. A causal relationship was suggested by the MR analysis between IQ and PD, but not between RHR and PD. RHR and IQ in late adolescence were associated with a higher risk of PD diagnosed at relatively young age. The association of IQ with PD is likely causal, whereas the association of RHR with PD suggests that altered cardiac autonomic function might start before 20 years of age in PD.
Related collections
Most cited references48

- Record: found
- Abstract: found
- Article: found
Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator

- Record: found
- Abstract: found
- Article: found
The MR-Base platform supports systematic causal inference across the human phenome

- Record: found
- Abstract: found
- Article: found