- Record: found
- Abstract: found
- Article: found
Exceedingly rare incidence of a double inferior vena cava (IVC) with azygos continuation of left IVC

Read this article at
Abstract
Key Clinical Message
Because of the complex embryonic origin of the abdominal venous structures, IVC and azygous systems can show numerous and even previously unreported anatomical variations and anomalies. Also, evaluating major vascular structures should not be dismissed in non‐contrast‐enhanced CT as it can provide valuable information about these structures.
Abstract
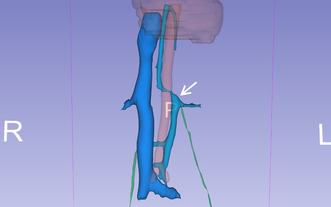
Double IVC is a rare occurrence of IVC anatomical variations and congenital anomalies. Herein, we discuss a case of a very rare type of double IVC that has not been reported in the literature before. A non‐contrast‐enhanced CT study was performed for a 34‐year‐old patient who visited our ER to evaluate for urolithiasis, during which two IVCs were noted. Each renal vein joined the ipsilateral IVC at a perpendicular angle. Unusually, the right IVC was formed from the confluence of both left and right common iliac veins (CIV), and the left IVC—Instead of crossing the midline at the renal veins level and reuniting the right IVC—cranially contributed to the azygos vein formation and caudally joined the left CIV. Also, there were some small communicating veins between the two IVCs and the left gonadal vein was slightly dilated before suggesting a reflux from the left renal vein (LRV). A complimentary doppler ultrasound exam confirmed the diagnosis and revealed a left‐side varicocele. Although rare cases of hemiazygos continuation and interiliac connections of left‐side IVC in the cases of double‐IVC have been reported previously, a complete confluence of CIVs is rare. The main differential diagnosis is retro‐aortic left renal vein (RLRV) type IV which seems to have an oblique course. Radiologists and surgeons should expect previously unreported variations in the vena cava system. Furthermore, reviewing the main abdominal vasculature should not be dismissed in non‐contrast CT exams.
Abstract
The operator assisted 3D reconstruction of the main retroperitoneal vasculature: the Aorta is shown in red; the right renal vein, right Inferior Vena Cava (IVC), and common iliac veins are depicted in dark blue; the left renal vein, left IVC, azygos vein, and accessory hemiazygos vein are illustrated in cyan; and the gonadal veins are represented in green. The left IVC exhibits multiple connections to the right IVC and the left Common Iliac Vein (CIV) caudally. It follows a vertical path and intersects with the left renal vein at a right angle. The superior segment of the left IVC, (arrow) does not merge with the right IVC after crossing the midline above the confluence of the left renal vein. Instead, it contributes to the formation of the azygos vein at the T12 vertebral level.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings.
- Record: found
- Abstract: found
- Article: not found
Inferior vena cava anomalies and variations: imaging and rare clinical findings
- Record: found
- Abstract: found
- Article: not found