- Record: found
- Abstract: found
- Article: found
Risk factors for relapse or persistence of bacteraemia caused by Enterobacter spp.: a case–control study
Read this article at
Abstract
Background
Enterobacter spp. possess chromosomal AmpC beta-lactamases that may be expressed at high levels. Previous studies have demonstrated a risk of relapsed bacteraemia following therapy with third generation cephalosporins (3GCs). What additional factors predict microbiological failure in Enterobacter bacteraemia is unclear. We aimed to determine factors associated with microbiological failure in Enterobacter bacteraemia.
Methods
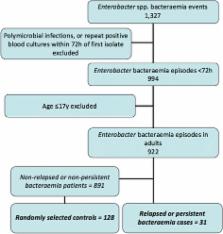
We retrospectively identified cases of bacteraemia caused by Enterobacter spp. occurring in four hospitals. Using a case–control design, we determined clinical risk factors for persistence or relapse defined as repeated positive blood cultures collected between 72 hours and up to 28 days post initial positive blood culture.
Results
During the study period a total of 922 bacteraemia events caused by Enterobacter spp. in adults were identified. The overall risk of relapsed or persisting bacteraemia at 28 days was low (31 of 922, 3.4%), with only 2 patients experiencing emergent resistance to 3GCs. A total of 159 patients were included in the case–control study. Using multivariate logistic regression, independent predictors for relapse were a line-associated source of infection (OR 3.87; 95% CI 1.56-9.60, p = 0.004) and the presence of immunosuppression (OR 2.70; 95% CI 1.14-6.44, p = 0.02). On univariate analysis definitive therapy with a broad-spectrum beta-lactam-beta-lactamase inhibitor (BLBLI, e.g. piperacillin-tazobactam) was not associated with relapse (OR 1.83; 95% CI 0.64-5.21, p = 0.26) although the proportion of patients receiving a BLBLI as definitive therapy was relatively small (21/159, 13.2%).
Conclusions
The risk of relapsed or persistent Enterobacter bacteraemia appears to be low in Australia. A line-associated source of infection and immunocompromise were significant independent predictors for relapse. Larger, preferably randomized, studies are needed to address whether BLBLIs represent an effective carbapenem-sparing option for Enterobacter bacteraemia.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Enterobacter spp.: pathogens poised to flourish at the turn of the century.
- Record: found
- Abstract: found
- Article: not found
Emergence of antibiotic resistance during therapy for infections caused by Enterobacteriaceae producing AmpC beta-lactamase: implications for antibiotic use.
- Record: found
- Abstract: found
- Article: not found