- Record: found
- Abstract: found
- Article: found
Risk factors for small-for-gestational-age and preterm births among 19,269 Tanzanian newborns
Read this article at
Abstract
Background
Few studies have differentiated risk factors for term-small for gestational age (SGA), preterm-appropriate for gestational age (AGA), and preterm-SGA, despite evidence of varying risk of child mortality and poor developmental outcomes.
Methods
We analyzed birth outcome data from singleton infants, who were enrolled in a large randomized, double-blind, placebo-controlled trial of neonatal vitamin A supplementation conducted in Tanzania. SGA was defined as birth weight <10th percentile for gestation age and sex using INTERGROWTH standards and preterm birth as delivery at <37 complete weeks of gestation. Risk factors for term-SGA, preterm-AGA, and preterm-SGA were examined independently using log-binomial regression.
Results
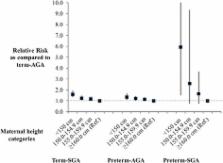
Among 19,269 singleton Tanzanian newborns included in this analysis, 68.3 % were term-AGA, 15.8 % term-SGA, 15.5 % preterm-AGA, and 0.3 % preterm-SGA. In multivariate analyses, significant risk factors for term-SGA included maternal age <20 years, starting antenatal care (ANC) in the 3 rd trimester, short maternal stature, being firstborn, and male sex (all p < 0.05). Independent risk factors for preterm-AGA were maternal age <25 years, short maternal stature, firstborns, and decreased wealth (all p < 0.05). In addition, receiving ANC services in the 1 st trimester significantly reduced the risk of preterm-AGA ( p = 0.01). Significant risk factors for preterm-SGA included maternal age >30 years, being firstborn, and short maternal stature which appeared to carry a particularly strong risk (all p < 0.05).
Conclusion
Over 30 % of newborns in this large urban and rural cohort of Tanzanian newborns were born preterm and/or SGA. Interventions to promote early attendance to ANC services, reduce unintended young pregnancies, increased maternal height, and reduce poverty may significantly decrease the burden of SGA and preterm birth in sub-Saharan Africa.
Trial registration
Australian New Zealand Clinical Trials Registry (ANZCTR) – ACTRN12610000636055, registered on 3 rd August 2010.
Related collections
Most cited references16

- Record: found
- Abstract: found
- Article: found
The associations of birth intervals with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis
- Record: found
- Abstract: found
- Article: not found
Advanced maternal age and adverse perinatal outcome: a review of the evidence.
- Record: found
- Abstract: found
- Article: not found