- Record: found
- Abstract: found
- Article: found
Intestinal Barrier Dysfunction, LPS Translocation, and Disease Development
Read this article at
Abstract
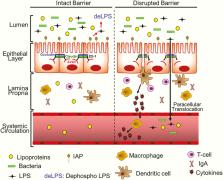
The intestinal barrier is complex and consists of multiple layers, and it provides a physical and functional barrier to the transport of luminal contents to systemic circulation. While the epithelial cell layer and the outer/inner mucin layer constitute the physical barrier and are often referred to as the intestinal barrier, intestinal alkaline phosphatase (IAP) produced by epithelial cells and antibacterial proteins secreted by Panneth cells represent the functional barrier. While antibacterial proteins play an important role in the host defense against gut microbes, IAP detoxifies bacterial endotoxin lipopolysaccharide (LPS) by catalyzing the dephosphorylation of the active/toxic Lipid A moiety, preventing local inflammation as well as the translocation of active LPS into systemic circulation. The causal relationship between circulating LPS levels and the development of multiple diseases underscores the importance of detailed examination of changes in the “layers” of the intestinal barrier associated with disease development and how this dysfunction can be attenuated by targeted interventions. To develop targeted therapies for improving intestinal barrier function, it is imperative to have a deeper understanding of the intestinal barrier itself, the mechanisms underlying the development of diseases due to barrier dysfunction (eg, high circulating LPS levels), the assessment of intestinal barrier function under diseased conditions, and of how individual layers of the intestinal barrier can be beneficially modulated to potentially attenuate the development of associated diseases. This review summarizes the current knowledge of the composition of the intestinal barrier and its assessment and modulation for the development of potential therapies for barrier dysfunction-associated diseases.
Related collections
Most cited references69

- Record: found
- Abstract: found
- Article: found
Intestinal Permeability in Inflammatory Bowel Disease: Pathogenesis, Clinical Evaluation, and Therapy of Leaky Gut
- Record: found
- Abstract: found
- Article: not found
Microbial modulation of innate defense: goblet cells and the intestinal mucus layer.
- Record: found
- Abstract: found
- Article: not found