- Record: found
- Abstract: found
- Article: found
Who is your prenatal care provider? An algorithm to identify the predominant prenatal care provider with claims data
Read this article at
Abstract
Background
Using claims data to identify a predominant prenatal care (PNC) provider is not always straightforward, but it is essential for assessing access, cost, and outcomes. Previous algorithms applied plurality (providing the most visits) and majority (providing majority of visits) to identify the predominant provider in primary care setting, but they lacked visit sequence information. This study proposes an algorithm that includes both PNC frequency and sequence information to identify the predominant provider and estimates the percentage of identified predominant providers. Additionally, differences in travel distances to the predominant and nearest provider are compared.
Methods
The dataset used for this study consisted of 108,441 live births and 2,155,076 associated South Carolina Medicaid claims from 2015–2018. Analysis focused on patients who were continuously enrolled throughout their pregnancy and had any PNC visit, resulting in 32,609 pregnancies. PNC visits were identified with diagnosis and procedure codes and specialty within the estimated gestational age.
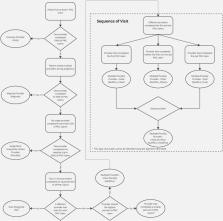
To classify PNC providers, seven subgroups were created based on PNC frequency and sequence information. The algorithm was developed by considering both the frequency and sequence information. Percentage of identified predominant providers was reported. Chi-square tests were conducted to assess whether the probability of being identified as a predominant provider for a specific subgroup differed from that of the reference group (who provided majority of all PNC). Paired t-tests were used to examine differences in travel distance.
Results
Pregnancies in the sample had an average of 7.86 PNC visits. Fewer than 30% of the sample had an exclusive provider. By applying PNC frequency information, a predominant provider can be identified for 81% of pregnancies. After adding sequential information, a predominant provider can be identified for 92% of pregnancies. Distance was significantly longer for pregnant individuals traveling to the identified predominant provider (an average of 5 miles) than to the nearest provider.
Related collections
Most cited references28

- Record: found
- Abstract: found
- Article: found
Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality
- Record: found
- Abstract: found
- Article: not found
An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index.
- Record: found
- Abstract: found
- Article: not found