- Record: found
- Abstract: found
- Article: found
Mycobacterial Pulmonary Infections in Patients with Idiopathic Pulmonary Fibrosis
Read this article at
Abstract
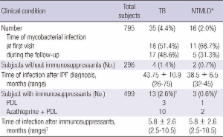
Patients with idiopathic pulmonary fibrosis (IPF) have an increased risk for developing tuberculosis (TB). However, no studies have been reported regarding the development of nontuberculous mycobacterium (NTM) lung disease (NTMLD). We reviewed 795 patients with IPF from five university hospitals who were diagnosed by histological or radio-clinical criteria. In the 795 patients with IPF, pulmonary infections with mycobacterium tuberculosis (MTB) and NTM were found in 35 (4.4%) and 16 patients (2.0%), respectively, which was a higher frequency than that found in the general population. TB was more common in patients treated with immunosuppressants than in those who did not receive immunosuppressants (2.6% vs 1.4%, P = 0.12). Among the IPF patients who had mycobacterial infections,immunosuppressant users developed TB or NTMLD within 1 yr after treatment with immunosuppressants,while those occurred later than 2 yr after diagnosis of IPF in the subjects that did not receive immunosuppressants. Among 51 IPF patients who had mycobacterial infections, 9 (18%) died during follow-up. Of these, three died due to progression of pulmonary tuberculosis. TB and NTMLD is relatively common in patients with IPF in Korea and may be fatal in some groups. Careful evaluation of TB and NTMLD is necessary not only for immunosuppressant users, but also for nonusers with IPF.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Idiopathic pulmonary fibrosis: prevailing and evolving hypotheses about its pathogenesis and implications for therapy.
- Record: found
- Abstract: found
- Article: not found