- Record: found
- Abstract: found
- Article: found
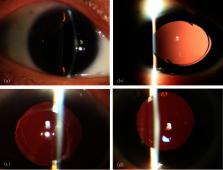
Flapless and Conjunctiva-Sparing Technique for Transscleral Fixation of Intraocular Lens to Correct Refractive Errors in Eyes without Adequate Capsular Support
Read this article at
Abstract
Purpose
To evaluate refractive outcomes, intraocular lens (IOL) power calculation, and IOL position following a novel conjunctiva-sparing transscleral fixation technique.
Methods
Forty-one eyes of 40 patients managed with a flapless transscleral-sutured technique were included. Preoperative and postoperative refractive errors (spherical equivalents, SE) were compared. IOL position was assessed on the Scheimpflug images. IOL power was calculated by SRK/T, Holladay 1, and Hoffer Q formulas.
Results
The mean age was 57.39 ± 14.83 years (range: 26 to 79 years), and the mean follow-up was 7.46 ± 6.42 months (range: 1 to 24 months). Surgical indications were aphakia ( n = 14), subluxated lenses ( n = 3), and IOL dislocation ( n = 24). The SE was 4.50 ± 6.38 diopter (D) (range: −3.75 to 13.75 D) preoperatively and −1.68 ± 1.57 D (range: −5.50 to 1.13 D) postoperatively ( P < 0.001). The mean tilt angle and decentration were 2.90° ± 1.93° (range: 0.39° to 9.10°) and 0.23 ± 0.19 mm (range: 0.02 to 0.94 mm) vertically, and 1.75° ± 1.41° (range: 0.24° to 7.65°) and 0.18 ± 0.19 mm (range: 0.02 to 1.06 mm) horizontally, which were clinically insignificant. All three IOL formulas produced myopic errors (range: −0.29 to −0.50 D). The SRK/T had the lowest median absolute error (0.55 D), followed by the Holladay 1 (0.70 D) and the Hoffer Q (0.74 D). The three formulas had the same percentage of prediction errors (PEs) within ±0.5 D (43.48%), while the Hoffer Q had the highest percentage of PEs within ±1.0 D (82.61%).
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
Flanged Intrascleral Intraocular Lens Fixation with Double-Needle Technique.
- Record: found
- Abstract: found
- Article: not found
Accuracy of Intraocular Lens Calculation Formulas.
- Record: found
- Abstract: found
- Article: not found