INTRODUCTION
A relatively common procedure often performed by junior-level staff, percutaneous central venous catheterization (CVC) is nevertheless associated with significant morbidity and mortality.(1–3) Percutaneous CVC is indicated for numerous reasons including long-term pharmacotherapy, haemodynamic monitoring, administration of medications likely to induce phlebitis, and failure to establish peripheral intravenous access.(1–4) The technique of central venous catheter insertion is dependent on a number of factors including the indication for the procedure, experience of the health care professional performing the procedure, and the clinical scenario encountered – for instance patient weight, history of previous catheterization and whether the procedure is performed under general anaesthesia or with the use of ultrasonography.(1–5) Complication rates for percutaneous CVC placement range from 0.7% to 23% in the international literature.(1) Complications can be classified as mechanical, thrombotic, and infectious. Mechanical complications such as arterial puncture, haemothorax, pneumothorax, air embolism, and catheter malposition are usually immediately apparent and are the most likely complications to require surgical intervention.(3,6) Complications with delayed presentation include catheter-related blood stream infection, venous thrombosis and embolism, catheter migration, and nerve injury.(5,7) Complication rates of paediatric CVC are dependent upon numerous factors including experience level of the individual performing the procedure, size of the child, clinical scenario in which the line is placed, and whether the procedure is done under ultrasound guidance or not.(3,5) Specific sites of CVC insertion, including the femoral, subclavian, and internal jugular veins, all carry their own unique advantages, disadvantages, and risks of complication.(7) Ultrasound-guided percutaneous CVC is now the gold standard technique and has demonstrably lower morbidity and mortality than traditional techniques that utilize external anatomical landmarks.(7–9)
Though well described within international literature, there is no local literature that has assessed the paediatric patient profile requiring CVCs, indications for CVCs, the techniques for central venous access, or the complications associated with line placement. This study is a first step in the process to develop strategies to decrease morbidity, mortality, and cost associated with CVC in the South African paediatric population.
METHODS
A prospective study was performed from 1 May to 31 July 2017, at Chris Hani Baragwanath Academic Hospital (CHBAH). Ethical clearance was obtained from the University of the Witwatersrand Human Research Ethics Committee. All patients in whom a central venous catheter was inserted by staff of the department of Paediatric Surgery were eligible for inclusion. Study participation was voluntary. All collected data remained anonymous and were obtained with written informed consent. Data collected included patient characteristics, indication for and technique of CVC, seniority level of medical professional performing CVC and immediate complications of CVC. Descriptive statistics were performed using Microsoft Excel. Analytic statistics were performed using the Fischer's Exact and Chi-squared tests. A P value <0.05 was considered significant.
RESULTS
Of the total 129 central venous catheters placed during the study period, data were collected on 95 insertions. The median age for patients requiring CVC was 60 days, with a range of 1–5760 days. The majority (78/95, 82%) of patients requiring CVC had underlying surgical pathology, with 44% (42/95) of CVC occurring in the intensive care unit, 29% (28/95) in the general wards, and 26% (25/95) in the operating theatre. A total of 43 (45%) patients had previous CVC insertion, of which 13 (14%) had more than 2 previous central venous catheters.
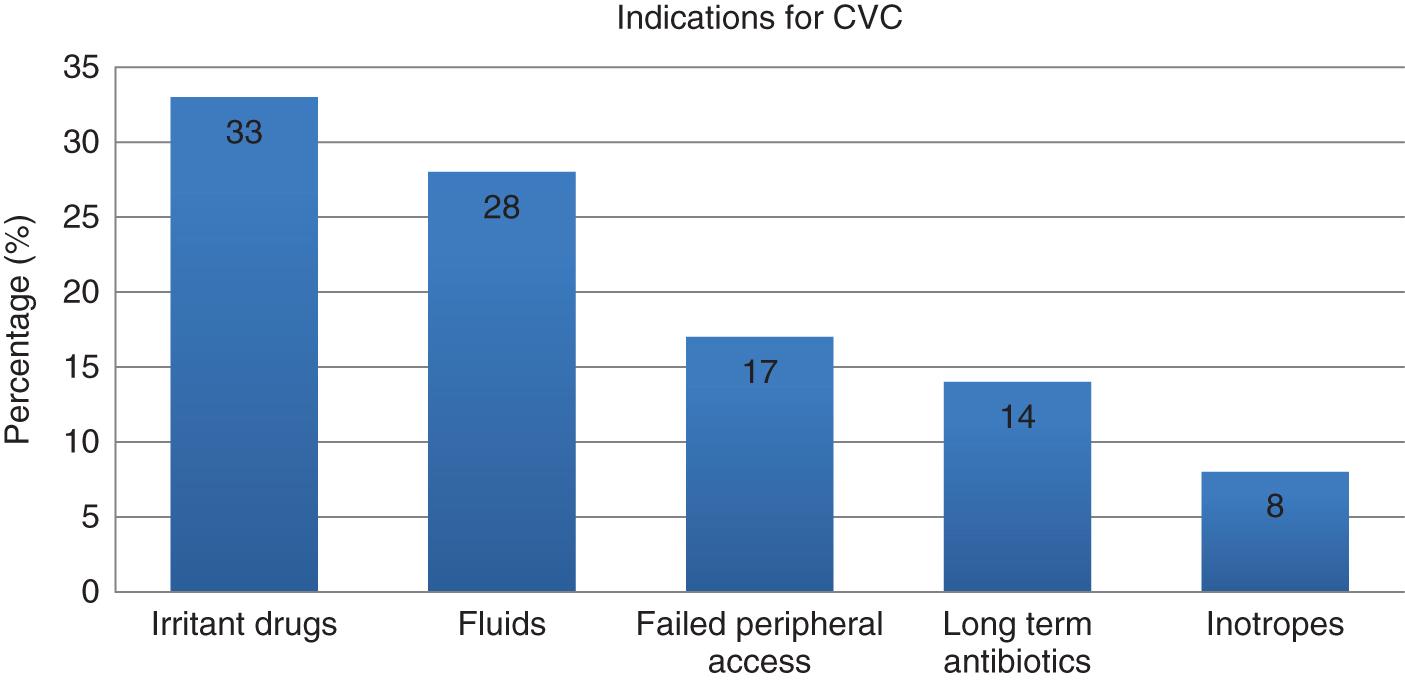
Irritant drugs (31/95, 33%), fluids (27/95, 28%), which included blood products and resuscitation fluids, and failure to establish peripheral intravenous access (16/95, 17%) were the most common indications for CVC. These data are presented in Figure 1.
The majority of CVC (54%, 51/95) were placed by paediatric surgical trainees, with the remainder placed by junior staff (medical officer or general surgical trainee on paediatric surgical rotation) (43%, 41/95) and paediatric surgical consultants (3%, 3/95). All CVCs were inserted percutaneously without ultrasound guidance. 55% (52/95) of patients were intubated at the time of CVC insertion. CVC placed in the neonatal unit accounted for 55% (52/95) of all line insertions. The remainder of line placements were accounted for by paediatric burns patients (27%, 26/95), emergency room and general medical and surgical patients (15%, 14/95) and patients in the paediatric intensive care unit (3%, 3/95). Frequency of CVC site is summarized in Figure 2.
A total of 12 (13%) immediate mechanical complications of CVC were reported. No deaths, haemothoraces or pneumothoraces associated with CVC were reported. The majority of catheter malposition (78%, 7/9) occurred when utilizing the subclavian veins. Summary data on mechanical CVC complications are presented in Table 1.
Mechanical complications of CVC insertion
| Insertion-related complications (n=12) | |
| Malposition | 9 |
| Arterial puncture | 2 |
| Failed insertion | 1 |
No statistical difference (P < 0.05) was found in complication rates between line placement by junior staff (medical officer or general surgical trainee) and senior staff (paediatric surgical trainee or consultant), between subclavian and internal jugular CVC, between patients with previous central venous access and those without, and between intubated and awake patients. Summary data are presented in Table 2.
Comparative analysis of complications associated with line placement
| Complicated | Uncomplicated | ||
|---|---|---|---|
| Junior | 7 (7.4%) | 33 (34.7%) | P = 0.19 |
| Senior | 5 (5.3%) | 50 (52.6%) | |
| Subclavian | 10 (11.9%) | 69 (82.1%) | P = 0.13 |
| Internal jugular | 1 (1.2%) | 4 (4.8%) | |
| Previous CVC | 8 (8.4%) | 35 (36.8%) | P = 0.51 |
| No previous CVC | 4 (4.3%) | 48 (50.5%) | |
| Intubated | 5 (5.3%) | 47 (49.5%) | P = 0.34 |
| Awake | 7 (7.3%) | 36 (37.9%) |
DISCUSSION
CVC is a frequent procedure in the paediatric population. Complications of CVC may be classified as mechanical, thrombotic, or infectious.(1–3,6,7) Reported rates of mechanical complication within existing literature are wide, ranging from 2% to 25%.(6) Experience level of the health care practitioner performing CVC, age of the patient, use of ultrasound, and previous CVC attempts have all been found to significantly impact upon the risk for mechanical complications requiring intervention.(1,3,7) The mechanical complication rate in our series was 13%. We did not find any statistical difference in complication rates based on level of experience of healthcare worker performing CVC, site of insertion, whether patients were ventilated or breathing spontaneously, and between patients with previous CVC and those without. Catheter malposition was the most common complication, followed by arterial puncture, and failure to establish central venous access.
It is revealing that there were no significant differences in the complication rates of CVC between junior and senior surgical staff. Junior staff within the department are taught the indications for, technique and complications of, and management of complications of CVC insertion as part of ‘on the job’ training by more senior staff before attempting this procedure. The lack of a statistically significant difference in the rate of complications between junior and senior staff may be explained by the small sample size in our study, but it may also suggest that with appropriate training, non-surgical staff, including paediatricians, anaesthetists, intensivists, and nurse practitioners may safely be trained in paediatric CVC in our setting. Internationally, paediatric central venous access is performed by a wide range of medical and allied health practitioners from paediatric intensivists and interventional radiologists to paediatric nurse practitioners.(7,10) Given the immense workload of the Department of Paediatric Surgery at CHBAH, and the fact that CVC should be a basic competence of medical professionals, the above findings support greater involvement of non-surgical staff in paediatric CVC and its alternatives in the local setting.
Median age for patients requiring CVC was 60 days with a range from 1 to 5760 days. More than half (55%) of all CVC occurred in the neonatal unit, approximately half (45%, 43/95) of all patients with central venous catheters had at least one previous CVC, and 1 in every 7 patients had 2 or more previous central venous catheters. The high proportion of infants and neonates requiring CVC, and the number of patients with multiple previous CVC necessitates the use of alternative techniques for long-term intravenous access in addition to efforts for improved line care in our setting. Neonatal umbilical vein catheters and peripherally inserted central catheters (PICCs) are two such options. PICC lines afford the same long-term benefits as central venous catheters without the same risk of devastating complications and need for sedation or general anaesthesia, and may be performed by appropriately trained auxiliary staff such as nurses in the ward setting.(10)
Internationally, dedicated services for CVC and PICC insertion exist within major children's hospitals.
The most common reasons for CVC were administration of irritant drugs, delivery of intravenous fluids, and failure to establish peripheral intravenous access. Curiously, delivery of inotropes was the least common indication for central venous access. The argument for alternative forms of long-term intravenous access, and improved line care, is further supported by the fact that approximately 20% of CVCs were placed as a result of failure to establish peripheral access, and that 45% of patients required more than 1 CVC. The most common anatomical site for central line placement was the subclavian vein, followed by the femoral, and lastly internal jugular veins. This finding may be explained by the length and calibre of central venous catheters currently available in our facility and that the majority of CVC occurred in neonates and infants. Significantly, no CVC was placed under ultrasound guidance and less than one-third (26%) occurred within the operating theatre. High demand for CVC, a lack of theatre time to meet the immense demand, and a lack of infrastructure to perform ultrasound-guided CVC all contribute to these findings. CVC in the operating theatre under ultrasound guidance is considered the international gold standard in order to minimize the mechanical, thrombotic, and infectious complications associated with CVC.(7–9) The environment of the operating room and use of ultrasound offer the advantages of an appropriately positioned, still patient, in a sterile environment with an instrument proven to decrease the complications of CVC. Promotion of alternate techniques for long-term intravenous access, and provision of the resources for and training in ultrasound-guided CVC, may significantly reduce demand for CVC and complication rates of CVC in the local setting.
LIMITATIONS
This was a prospective study performed by means of convenience sampling at a single institution over a three-month period. The study was further limited by the sample size, sample distribution over time, sole focus on immediate mechanical complications of CVC and gaps in data collection resulting in only 74% (95/129) of potential study participants being included in the final study analysis. Given the small sample size, analytical statistics may have been prone to type II errors.
CONCLUSIONS AND RECOMMENDATIONS
The majority of CVC in our setting occurred in the neonatal unit, without the use of ultrasound guidance, outside of the setting of the operating theatre. Complication rates for mechanical complications fell within the range reported internationally. The high number of lines placed necessitates the establishment of a line service that identifies those patients at high risk of requiring CVC early, relieves the paediatric surgical service of the high burden of CVC, and actively pursues safer alternative avenues to CVC including ultrasound-guided insertion and PICC lines. Long-term studies that include the infectious and thrombotic complications of CVC are required in order to gain a more accurate understanding of the morbidity and cost of CVC in the local setting.