- Record: found
- Abstract: found
- Article: found
An umbrella review of systematic reviews on the impact of the COVID-19 pandemic on cancer prevention and management, and patient needs
Read this article at
Abstract
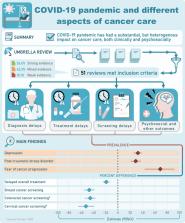
The relocation and reconstruction of health care resources and systems during the coronavirus disease 2019 (COVID-19) pandemic may have affected cancer care. An umbrella review was undertaken to summarize the findings from systematic reviews on impact of the COVID-19 pandemic on cancer treatment modification, delays, and cancellations; delays or cancellations in screening and diagnosis; psychosocial well-being, financial distress, and use of telemedicine as well as on other aspects of cancer care. Bibliographic databases were searched for relevant systematic reviews with or without meta-analysis published before November 29th, 2022. Abstract, full- text screening, and data extraction were performed by two independent reviewers. AMSTAR-2 was used for critical appraisal of included systematic reviews. Fifty-one systematic reviews were included in our analysis. Most reviews were based on observational studies judged to be at medium and high risk of bias. Only two reviews had high or moderate scores based on AMSTAR-2. Findings suggest treatment modifications in cancer care during the pandemic versus the pre-pandemic period were based on low level of evidence. Different degrees of delays and cancellations in cancer treatment, screening, and diagnosis were observed, with low- and- middle- income countries and countries that implemented lockdowns being disproportionally affected. A shift from in-person appointments to telemedicine use was observed, but utility of telemedicine, challenges in implementation and cost-effectiveness in cancer care were little explored. Evidence was consistent in suggesting psychosocial well-being of patients with cancer deteriorated, and cancer patients experienced financial distress, albeit results were in general not compared to pre-pandemic levels. Impact of cancer care disruption during the pandemic on cancer prognosis was little explored. In conclusion, substantial but heterogenous impact of COVID-19 pandemic on cancer care has been observed.
eLife digest
The onset of the COVID-19 pandemic disrupted many aspects of human life, not least healthcare. As resources were redistributed towards the crisis, social isolation rules also limited access to medical professionals. In particular, these measures may have affected many aspects of cancer care, such as early detection or treatment.
Many studies have aimed to capture the impact of these changes, but most have been observational, with researchers recording events without trying to impose a controlled design. These investigations also often faced limitations such as small sample sizes, or only focusing on one aspect of cancer care. Systemic reviews, which synthetize and assess existing research on a topic, have helped to bypass these constraints. However, they are themselves not devoid of biases. Overall, a clear, unified picture of the impact of COVID-19 on cancer care is yet to emerge.
In response, Muka et al. carried an umbrella analysis of 51 systematic reviews on this topic. They used a well-known critical appraisal tool to assess the methodological rigor of each of these studies, while also summarising their findings. This work aimed to capture many aspects of the patients’ experience, from diagnosis to treatment and the financial, psychological, physical and social impact of the disease.
The results confirmed that the pandemic had a substantial impact on cancer care, including delays in screening, diagnosis and treatment. Throughout this period cancer patients experienced increased rates of depression, post-traumatic stress and fear of their cancer progressing. The long-term consequences of these disruptions remain to be uncovered.
However, Muka et al. also showed that, overall, these conclusions rely on low-quality studies which may have introduced unaccountable biases. In addition, their review highlights that most of the data currently available has been collected in high- and middle-income countries, with evidence lacking from regions of the world with more limited resources.
In the short-term, these results indicate that interventions may be needed to mitigate the negative impact of the pandemic on cancer care; in the long-term, they also demonstrate the importance of rigorous systematic reviews in guiding decision making. By shining a light on the ripple effects of certain decisions about healthcare resources, this work could also help to shape the response to future pandemics.
Related collections
Most cited references65
- Record: found
- Abstract: not found
- Article: not found
Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses.
- Record: found
- Abstract: found
- Article: found
AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both

- Record: found
- Abstract: found
- Article: found