Transcatheter aortic valve implantation (TAVI) has emerged as the primary treatment strategy for severe symptomatic aortic stenosis (AS) in the older population (>75 years of age) with high-risk surgical profiles [1].
The growing older population and the concomitant age-related high prevalence of degenerative AS, combined with evidence of the non-inferiority of the TAVI procedure over surgical aortic valve replacement in intermediate-risk patients, increase the potential number of TAVI candidates. Concerns regarding the higher costs of TAVI than surgical aortic valve replacement are balanced by its shorter length of hospitalization and lower acute complication costs. However, the growing use of such treatment should lead to changes in the patient selection paradigm. Several studies have outlined the prognostic benefits of the procedure and identified independent negative factors. Among others, mitral regurgitation (MR) is frequently detected in patients diagnosed with AS. Improvements in MR after aortic valve stenosis surgical correction have been demonstrated. Nevertheless, the literature has described discordant results, with better results for functional MR than degenerative MR after TAVI [2, 3]. The pre-operative presence of degenerative MR can affect prognosis after TAVI and serves as independent factor in worsening overall cardiac function. Solely grading degenerative MR does not enable proper stratification of patients according to their heart function and may be the reason for the discordant results. How can TAVI candidates affected by degenerative MR be correctly stratified to avoid poor postoperative prognosis?
| What is the scientific question being addressed? |
| How can TAVI candidates affected by degenerative MR be correctly stratified to avoid poor postoperative prognosis? |
| What is the main novel finding? |
| New classification systems based on extra-valvular cardiac involvement may help in this aim. |
The staging analysis of patients with MR and AS must be framed with a focus on the pathophysiology and natural history of the valvular diseases, to achieve a better prognostic understanding. New classification systems based on extra-valvular cardiac involvement may help in this aim. In particular, our study was aimed at assessing the prognostic effects of degenerative MR (≥ 2+ according to Van Wijngaarden’s classification system) [4] in patients who underwent TAVI at our center. We analyzed mortality at follow-up (average time of 30.66 months) according to the MR staging. Interestingly, advanced extra-valvular involvement influenced prognosis after TAVI. Patients with degenerative MR grade ≥ 2 and right ventricle or tricuspid valve involvement showed a 2-year mortality of 50% after TAVI (Figure 1), which might not justify the procedural costs.
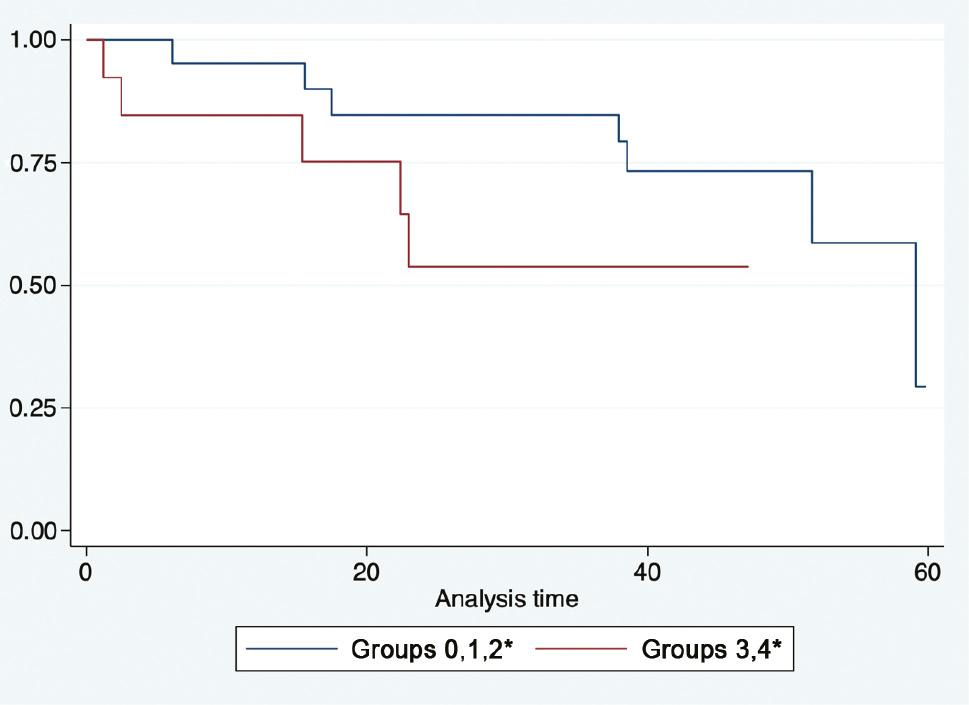
Kaplan-Meier Survival Estimates of Patients who Underwent TAVI with Preoperative Diagnosis of Degenerative Mitral Regurgitation ≥2+. MR is staged in groups according to extra-mitral valve cardiac involvement. Groups 0, 1, and 2, and groups 3 and 4 were analyzed together*.
*Group 0: no extra-mitral valve cardiac involvement. Group 1: LVESVi ≥ 30 mL/m2 or LVEF ≤ 60%. Group 2: history of AF. Group 3: TR grade > 2 or SPAP > 50 mmHg. Group 4: TAPSE ≤ 17 mm. HR: 2.55, range: 0.721/9.079; P value = ns.
Indeed, in 36 patients who underwent TAVI and were diagnosed with significant preoperative degenerative MR, we performed Kaplan-Meier analysis for various subsets of patients and observed a divergent mortality plot, even though no statistical significance was identified. In performing the same analysis in two groups, on the basis of right ventricle involvement, and analyzing groups 0, 1, and 2, and groups 3 and 4 together, we found that patients with right chamber involvement had poorer outcomes than those with isolated left pathology, even though the findings were not statistically significant (Figure 1) (HR: 2.55, range: 0.721/9.079, P value: ns). We used Van Wijngaarden’s staging system [4] to divide our 36 patients into five groups.
The involvement of the right cardiac chambers with the presence of degenerative MR grade ≥ 2 was associated with a 2.5-fold elevated risk of death after TAVI, even though the finding was not statistically significant, probably because of the small sample size.
Degenerative MR with grade ≥ 2 may be an important factor leading to poor outcomes and might accelerate the impairment in overall heart function. The discordant results published in the literature might reflect insufficient MR stratification. The staging classification may be considered to fully understand the influence of significant degenerative MR in patients eligible for TAVI. The role of extra-valvular involvement has been confirmed by the literature.
Indeed, Nishida and colleagues [5] have demonstrated that, among the prognostic factors potentially affecting TAVI outcomes, atrial fibrillation and the Society of Thoracic Surgeons score are associated with all-cause mortality in the male population. Moreover, Baz and colleagues [3], in an analysis of the effects of mitral and tricuspid regurgitation in patients who underwent TAVI, have found several predictors of 2-year mortality, including atrial fibrillation, relevant TR, and systolic pulmonary artery pressure.
In another study by Amat-Santos and colleagues [2], the presence of moderate MR did not influence short- and mid-term mortality post-TAVI, despite being associated with more rehospitalizations; however, the presence of moderate or severe TR was associated with higher mortality.
The extra-mitral valve involvement staging classification may significantly influence the proper stratification of patients affected by degenerative MR eligible for TAVI. Therefore, at least among patients with elevated risk, further study of degenerative MR of grade ≥ 2 and right ventricle disfunction, among other factors, may be necessary to assess the benefits of the procedure. Further studies will be essential to improve the selection of patients eligible for TAVI.
