- Record: found
- Abstract: found
- Article: found
Association between comprehensive geriatric assessment and short-term outcomes among older adult patients with stroke: A nationwide retrospective cohort study using propensity score and instrumental variable methods
Read this article at
Abstract
Background
Comprehensive geriatric assessment (CGA) is a multidimensional and multidisciplinary method to identify geriatric conditions among older patients. The aim of the present study was to examine the associations between CGA and short-term outcomes among older adult inpatients with stroke.
Methods
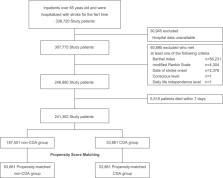
The study was a nationwide, retrospective cohort study. We used the Diagnosis Procedure Combination database, a national Japanese inpatient database, to identify older adult stroke patients from 2014 to 2017. The associations between CGA and in-hospital mortality, length of hospital stay, readmission rate, rehabilitation intervention, and introduction of home health care were evaluated using propensity score matching and instrumental variable analysis.
Findings
We identified 338,720 patients, 21·3% of whom received CGA. A propensity score-matched analysis of 53,861 pairs showed that in-hospital mortality was significantly lower in the CGA group than in the non-CGA group (3·6% vs. 4·1%, p < 0·001). The rate of long-term hospitalization (> 60 days) was significantly lower in the CGA group than in the non-CGA group (8·7% vs. 10·1%, p < 0·001), and the rates of rehabilitation intervention (30·3% vs. 24·9%, p < 0·001) and home health care (8·3% vs. 7·6%, p = 0·001) were both higher in the CGA group than in the non-CGA group. Instrumental variable analysis showed similar results.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Two-stage residual inclusion estimation: addressing endogeneity in health econometric modeling.

- Record: found
- Abstract: found
- Article: found
Comparing paired vs non-paired statistical methods of analyses when making inferences about absolute risk reductions in propensity-score matched samples
- Record: found
- Abstract: found
- Article: not found