- Record: found
- Abstract: found
- Article: found
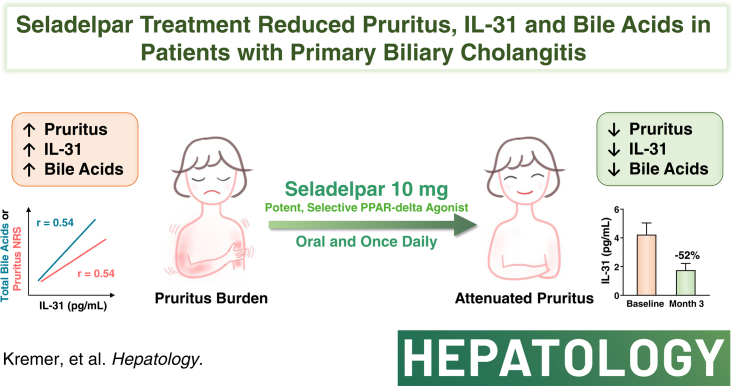
Seladelpar treatment reduces IL-31 and pruritus in patients with primary biliary cholangitis

Read this article at
Abstract
Background and Aims:
Pruritus is a debilitating symptom for many people living with primary biliary cholangitis (PBC). In studies with seladelpar, a selective peroxisome proliferator-activated receptor-delta agonist, patients with PBC experienced significant improvement in pruritus and reduction of serum bile acids. Interleukin-31 (IL-31) is a cytokine known to mediate pruritus, and blocking IL-31 signaling provides relief in pruritic skin diseases. This study examined the connection between seladelpar’s antipruritic effects and IL-31 and bile acid levels in patients with PBC.
Approach and Results:
IL-31 levels were quantified in serum samples from the ENHANCE study of patients with PBC receiving daily oral doses of placebo (n = 55), seladelpar 5 mg (n = 53) or 10 mg (n = 53) for 3 months, and for healthy volunteers (n = 55). IL-31 levels were compared with pruritus using a numerical rating scale (NRS, 0–10) and with bile acid levels. Baseline IL-31 levels closely correlated with pruritus NRS ( r = 0.54, p < 0.0001), and total ( r = 0.54, p < 0.0001) and conjugated bile acids (up to 0.64, p < 0.0001). Decreases in IL-31 were observed with seladelpar 5 mg (−30%, p = 0.0003) and 10 mg (−52%, p < 0.0001) versus placebo (+31%). Patients with clinically meaningful improvement in pruritus (NRS ≥ 2 decrease) demonstrated greater dose-dependent reductions in IL-31 compared to those without pruritus improvement (NRS < 2 decrease). Strong correlations were observed for the changes between levels of IL-31 and total bile acids ( r = 0.63, p < 0.0001) in the seladelpar 10 mg group.
Abstract
Related collections
Most cited references40
- Record: found
- Abstract: found
- Article: not found
A Placebo-Controlled Trial of Obeticholic Acid in Primary Biliary Cholangitis
- Record: found
- Abstract: not found
- Article: not found
Primary Biliary Cholangitis: 2018 Practice Guidance from the American Association for the Study of Liver Diseases
- Record: found
- Abstract: found
- Article: not found