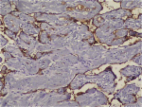
Background Intravascular papillary endothelial hyperplasia (IPEH) is a benign intravascular process with features mimicking other benign and malignant vascular proliferations. IPEH lesions predominate in the head-neck region and the extremities. The characteristic histomorphological feature of IPEH is a papillary structure covered with hyperplastic endothelial cells within the vascular lumen. It is critical that this clinically benign lesion should not be mistaken for well-differentiated vascular tumors. In addition to the characteristic histological features, other useful diagnostic features included the intra-luminal location of the lesion, an intimate association with the organizing thrombus, the absence of necrosis, cellular pleomorphism, and mitotic activity. In addition, immunohistochemistry may indicate the vascular origin and proliferative index. In this study, we evaluated histomorphological and immunohistochemical findings (CD31, CD34, FVIII, type IV collagen, SMA, MSA, CD105, and Ki-67 staining) of ten IPEH cases. Methods Ten IPEH cases were re-examined for a panel of histomorphological and immunohistochemical features. CD31, CD34, FVIII, Type IV collagen, SMA and MSA antibodies utilized for immunohistochemical analysis. The histomorphological and immunohistochemical findings were evaluated by two independent pathologists using light microscopy. Results All ten cases involved intraluminal lesions with characteristic features of IPEH. All ten cases (100%) were stained positive for CD31 and CD34. The degree of staining with FVIII, type IV collagen, SMA, and MSA was variable. Conclusion In this series of specimens, CD31 and CD34 were the most sensitive markers indicating the vascular origin of the lesion. Staining for the other vascular markers (FVIII, type IV collagen, SMA and MSA) was variable. Different maturation degrees of lesions may account for the variation in immunohistochemical staining. Few previous investigations evaluated a wide range of antigen panels in IPEH sections. In our opinion, the evaluation of immune markers in a larger sample set will reveal new features in the maturity and developmental pathogenesis of vascular lesions and angiogenesis. IPEH is a benign lesion, which must be differentiated from malignant tumors such as angiosarcoma and Kaposi’s sarcoma. Improved definition of IPEH lesions using immunohistochemical markers may enhance the ability to differentiate between various vascular lesions. Virtual slides The virtual slide(s) for this article can be found here: http://www.diagnosticpathology.diagnomx.eu/vs/1381849312101856.