- Record: found
- Abstract: found
- Article: found
Fixation-induced surgical segment’s high stiffness and the damage of posterior structures together trigger a higher risk of adjacent segment disease in patients with lumbar interbody fusion operations
Read this article at
Abstract
Background
Adjacent segment disease (ASD) is a commonly reported complication after lumbar interbody fusion (LIF); changes in the mechanical environment play an essential role in the generation of ASD. Traditionally, fixation-induced high stiffness in the surgical segment was the main reason for ASD. However, with more attention paid to the biomechanical significance of posterior bony and soft structures, surgeons hypothesize that this factor may also play an important role in ASD.
Methods
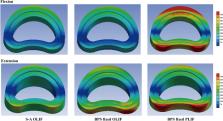
Oblique and posterior LIF operations have been simulated in this study. The stand-alone OLIF and OLIF fixed by bilateral pedicle screw (BPS) system have been simulated. The spinal process (the attachment point of cranial ligamentum complex) was excised in the PLIF model; the BPS system has also been used in the PLIF model. Stress values related to ASD have been computed under physiological body positions, including flexion, extension, bending, and axial rotations.
Results
Compared to the stand-alone OLIF model, the OLIF model with BPS fixation suffers higher stress values under extension body position. However, there are no apparent differences under other loading conditions. Moreover, significant increases in stress values can be recorded in flexion and extension loading conditions in the PLIF model with posterior structures damage.
Conclusions
Fixation-induced surgical segment’s high stiffness and the damage of posterior soft tissues together trigger a higher risk of ASD in patients with LIF operations. Optimizing BPS fixation methods and pedicle screw designs and reducing the range of posterior structures excision may be an effective method to reduce the risk of ASD.
Related collections
Most cited references56
- Record: found
- Abstract: found
- Article: not found
Magnetic resonance classification of lumbar intervertebral disc degeneration.
- Record: found
- Abstract: found
- Article: not found
What is intervertebral disc degeneration, and what causes it?
- Record: found
- Abstract: found
- Article: not found