- Record: found
- Abstract: found
- Article: found
Five-year mortality in a cohort of people with schizophrenia in Ethiopia
Read this article at
Abstract
Background
Schizophrenia is associated with a two to three fold excess mortality. Both natural and unnatural causes were reported. However, there is dearth of evidence from low and middle income (LAMIC) countries, particularly in Africa. To our knowledge this is the first community based report from Africa.
Methods
We followed a cohort of 307 (82.1% males) patients with schizophrenia for five years in Butajira, rural Ethiopia. Mortality was recorded using broad rating schedule as well as verbal autopsy. Standardized Mortality Ratio (SMR) was calculated using the mortality in the demographic and surveillance site as a reference.
Result
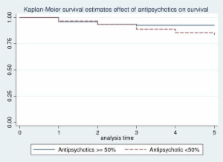
Thirty eight (12.4%) patients, 34 men (11.1%) and 4 women (1.3%), died during the five-year follow up period. The mean age (SD) of the deceased for both sexes was 35 (7.35). The difference was not statistically significant (p = 0.69). It was 35.3 (7.4) for men and 32.3 (6.8) for women. The most common cause of death was infection, 18/38 (47.4%) followed by severe malnutrition, 5/38 (13.2%) and suicide 4/38 (10.5%). The overall SMR was 5.98 (95% CI = 4.09 to7.87). Rural residents had lower mortality with adjusted hazard ratio (HR) of 0.30 (95% CI = 0.12-0.69) but insidious onset and antipsychotic treatment for less than 50% of the follow up period were associated with higher mortality, adjusted HR 2.37 (95% CI = 1.04-5. 41) and 2.66(1.054-6.72) respectively.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Suicide as an outcome for mental disorders. A meta-analysis.
- Record: found
- Abstract: not found
- Article: not found
Causes of the excess mortality of schizophrenia.
- Record: found
- Abstract: not found
- Article: not found