INTRODUCTION
Menstruation is a natural cyclical event that happens to women, and the period of menstruation is characterized by physical and emotional changes ( Sarwar and Rauf, 2021). Changes occur in a woman’s body during menstruation, and there are fluctuations in hormones. This makes her to face different feelings. Many women undergo changes in their bodies or moods, such as depression or weight gain ( Zaka and Mahmood, 2012; Gao et al., 2022). The symptoms get worse during the second half of the menstrual cycle and then fade and go away after the start of the next menstrual cycle. Some women may benefit from general health advice such as eating a balanced diet, reducing caffeine intake, and exercising regularly to stay fit ( Ne’ma, 2019).
Women often hide these effects and suffer silently, but there are many natural ways to reduce menstrual pain and premenstrual syndrome (PMS). They are related to the changes in hormone levels during women’s menstrual cycle. Severe PMS affects the woman’s life and work and hinders her from carrying out her duties during the days preceding the occurrence of menstruation ( Ne’ma, 2019).
The start of the PMS, which significantly affects aspects of daily life, is the most hated time by most women; the symptoms include feeling bloated, cramps, and mood swings; the menstrual cycle is the biggest obstacle at the level of daily life ( Schoep et al., 2019; Alshdaifat et al., 2022; Lee et al., 2022).
Hussein (2019) claims that 85% of females suffer monthly from symptoms of menstruation, and 5-10% of them are affected by these symptoms to the extent of complete disruption in their personal and professional lives. The suffering resulting from symptoms of menstruation leads to damage to the family environment. In severe cases, a woman may lose her relationship with the people closest to her, causing confusion and turmoil in the family atmosphere ( Hussein, 2019). It damages the social environment, and the educational, cultural, occupational, and health levels. It also leads to an economic burden due to the lack of production and the costs of medical care related to purchasing analgesic drugs or hospital admissions, etc. ( Ne’ma, 2019). It is interesting to note that there is an increase in the rates of hospital admissions, accidents, crimes, and suicide in the premenstrual period when women are in a state of high psychological sensitivity ( Lee et al., 2022).
Malhotra et al. (2020) found that women experience PMS and premenstrual dysphoric disorder (PMDD). Aşcı et al. (2015) found that the prevalence in Turkish studies was between 5 and 79%. Women’s physical and psychological lives are negatively affected by PMS. The severity of PMS in Saudi Arabia was as follows: 45% mild, 32.6% moderate, and 22.4% severe ( Balaha et al., 2010). The prevalence of PMS among college students in India ranged from 18.4 to 37% ( Buddhabunyakan et al., 2017). Other researchers (e.g. Enkhjargal et al., 2022; Rezende et al., 2022) showed the prevalence of moderate to severe PMS and PMDD among Mongolian and Brazilian people.
A group of factors affect menstruation, such as puberty, the duration of menstruation and its quantity, women’s weight gain, the number of pregnancies for married women, and maintaining body cleanliness ( Hussein, 2019).
To be diagnosed with the PMS—according to the diagnostic and statistical manual of mental disorders, Fifth Edition (DSM-5) ( American Psychiatric Association, 2013; Maity et al., 2022), at least one of the following symptoms should be present: significant emotional instability (example.g., mood swings: a sudden feeling of sadness and crying or increased sensitivity to rejection), marked restlessness or anger, increased interpersonal conflict, marked office mood, feeling hopelessness, increased thoughts of self-deprecation ( Nour et al., 2009; Laksham et al., 2019), marked anxiety and tension ( American Psychiatric Association, 2013), or feelings of being restricted.
In addition to the above at least one of the following should be present: decreased interest in usual activities, easy tiredness, feeling confused or out of control physical symptoms, such as tension or swollen breasts ( Hillard and Deitch, 2005), feeling bloated, or weight gain. These symptoms are accompanied by a significant decrease in mental state or interference with work, academics, social activities, or relationships with others (such as being away from social activities and inability to be effective at work ( Delara et al., 2012; American Psychiatric Association, 2013).
Some studies have proven that about 80% of the world’s women in the age of puberty and childbearing have experienced some of these feelings and psychological symptoms associated with their period. Usually, these symptoms are mild or moderate ( Hamid, 2012). The woman does not need medical treatment but needs support from those around her. Like any natural event, she accepts this event as a necessity for life and reproduction and is part of the many biological cycles that occur in humans ( Abul-Azeem, 2010, p. 24).
However, there are cases in which premenstrual symptoms appear severe and profound ( Hamid, 2012), as some women suffer from symptoms before and during menstruation to the degree that affects their ability to work and achieve and affects the quality of their life and social activities to the degree that rises to the level of a disease, which occurs periodically and for several days every month ( Abul-Azeem, 2010). This is what is indicated by a study ( Farrell and Slade, 1999) that 85% of females suffer monthly from the symptoms of menstruation syndrome, and 5-10% of them are affected by these symptoms to the point of complete disruption in their personal and professional lives.
Also, the suffering resulting from the symptoms of menstruation syndrome leads to damage to the family environment ( Al-Hassani, 2008, p. 44). In severe cases, the woman may lose her relationship with the closest people to her and cause confusion and disturbance in the family atmosphere ( Hamid, 2012, p.11). It also leads to damage to the social environment and the educational, cultural, educational, occupational, and health levels and the consequent economic burden due to the lack of production and the costs of medical care described in the purchase of palliative medicines or hospitalization, etc. ( Al-Hassani, 2008, p. 63). There is an increase in the rates of hospitalizations, accidents, crime, and suicide in the premenstrual period when women are in a state of high psychological sensitivity.
As noted by Kabat-Zinn (1990), mindfulness helps the individual to “be attentive on purpose in the present moment” (p. 87). It is negatively associated with chronic pain, mood swings, and stress, and there is increasing evidence to suggest that practicing mindfulness can facilitate important health and psychological benefits, such as reduced anxiety and depression, improved relationships, increased self-esteem, and improved immune function ( West, 2008). This concept originated from ancient Buddhist meditation practices and focused on the present moment without judgment ( Yeung, 2013).
Two components of mindfulness were found. They were self-regulation of attention and adoption of a particular orientation toward one’s experiences ( Brown and Ryan, 2003; Bishop et al., 2004; Phan-Le et al., 2022).
It is the case where the mind is flexible and open to the new. It plays a major role in freedom from automatic thoughts and unhealthy behavioral habits. It promotes self-regulating behavior and subjective well-being, and mental alertness reduces adverse health outcomes ( Jennings and Jennings, 2013).
It is linked as a feature and practice to good mental health. This can be attributed to the fact that mental alertness increases the experiences of positive emotions ( Mandal et al., 2012), which causes results that benefit mental health in the long term. It also increases the individual’s focus on the present experience (the here and now) to enhance positive mood, facilitating recovery from negative emotional states and mitigating adverse physiological effects ( Yeung, 2013).
Mindfulness predicts well-being across varied conditions ( Lustyk et al., 2011). As indicated by Lustyk et al. (2011), the woman who gets a high score on mindfulness also gets low scores in premenstrual symptom reports. This means that mindfulness-based intervention is likely to reduce symptom severity among those women who suffer from PMS ( Lustyk et al., 2011). However, Tayel et al. (2018) indicated that only statistically significant relation was present between mindfulness and behavioral symptoms. However, no statistically significant relationships were found between mindfulness and the total score of premenstrual symptoms and the rest of the subscales of premenstrual symptoms.
It has been reported in the literature that the severity of PMS symptoms interferes with daily activities and significantly affects the QoL ( Tolossa and Bekele, 2014; Al-Shahrani et al., 2021). Lower PMS symptoms predict high QoL ( Jeong and Ahn, 2018).
In a study by Haywood et al. (2007), perfectionism and low levels of maternal support were associated with premenstrual (PM) symptoms. In addition, spousal and maternal social support moderated the impact of perfectionism on physical symptoms.
Nour et al. (2009) reported that PMS is associated with lower scores in health-related quality of life (HRQoL), and women with PMS are weaker in work productivity than women without PMS. Zaka and Mahmood (2012) indicated that women commonly complain about PMS, which may affect their QoL. Similarly, Delara et al. (2012) found that menstruation symptoms significantly impact women’s QoL. However, when a woman receives positive family support, she becomes intense enough in the face of illness. Issa et al. (2010) found that moderate/severe intensity correlated significantly between PMS and quality of life. Zaka and Mahmood (2012) reported that PMS is a commonly encountered complaint among women and may affect women’s QoL and reduce their occupational productivity.
Akbarzadeh et al. (2017) showed a significant correlation between PMS score, mental health, and all its dimensions except for social interactions. Moreover, anxiety and sleep disorders, with a frequency of 51.2%, were the most common mental disorders among the students.
Lan and Su (2019) measured the symptoms of PMS and explored the affecting factors and predictors in female students with disabilities. The factors affecting severe PMS were a gynecological disease, diet, family menstruation, uncomfortable history, irregularity, lifestyle, irregular diet, learning hassles, interpersonal hassles, and irregular exercise. The crucial predictors of the severity of PMS were interpersonal hassles, gynecological disease, and irregular exercise. The explained proportion of variance was 16.9%. At the same time, the affecting factors of the remission of PMS were the severity of PMS and acceptance of mindfulness, while the crucial predictors of the remission of PMS were the same. The explained proportion of variance was 67.3%.
Al-Batanony and Alnohairm (2014) showed that the burden of PMS/PMDD on HRQoL was on mental and emotional HRQoL domains besides the physical HRQoL domains as the students with PMS reported poorer HRQoL as measured by SF-36 than those without PMS.
Karpagavalli and Raj (2020) found that dietary and lifestyle factors such as consumption of sweets and lack of bodily activity were associated with PMS. PMS was positively significantly correlated with all domains of QoL and the total quality of life score ( Al-Shahrani et al., 2021).
The aim is to investigate the relationship between PMS and mindfulness and the mediating role of perceived social support (PSS) and HRQoL among deaf/hard-of-hearing women.
MATERIALS AND METHODS
The model
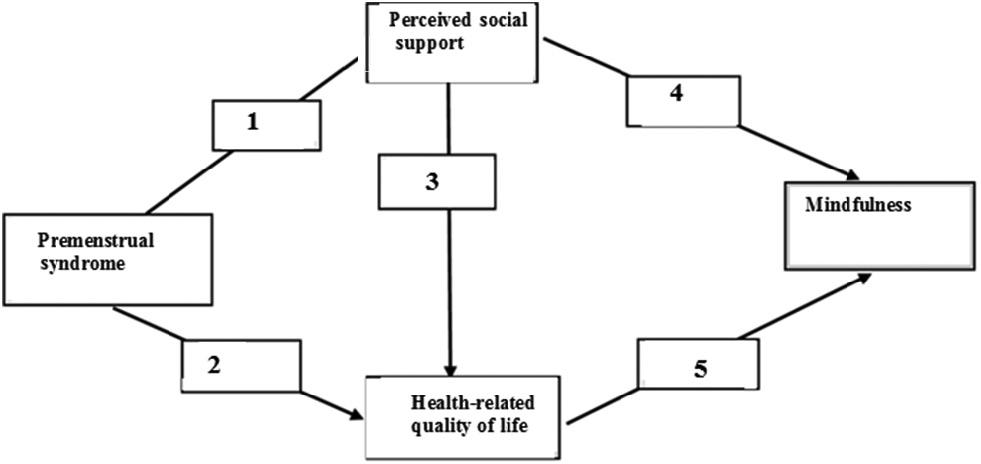
We test the relationship between PMS and mindfulness and the mediating role of PSS and HRQoL ( Fig. 1) in the model. We propose that PSS predicts HRQoL. In addition, we test PSS and HRQoL for their mediating effects between PMS and mindfulness.
Hypotheses
Research design
A cross-sectional, quantitative correlational study is proposed to investigate the relationship between PMS and mindfulness and the mediating role of PSS and HRQoL among deaf/hard-of-hearing women.
Participants
After explaining the purpose of the study, each participant signed and handed a written informed consent over to the researcher. Criteria for inclusion were as follows: (1) the age should be ≤18, (2) unmarried, and (3) living in Tabuk City, Kingdom of Saudi Arabia. Criteria for exclusion were as follows: any current medical or psychiatric disorders. Sixteen were excluded, not because these criteria were applied, but because they refused to be included in the study. A sample of 202 participants was selected. The study was conducted between December 2021 and March 2022.
Data collection instruments
PMS Scale ( Algahtani and Jahrami, 2014), a 23-question scale that assesses the prevalence and severity of PMS symptoms, was used. Each category’s questions for each individual were calculated by its mean score, for which the composite score was extracted. The Cronbach’s value for the whole questionnaire was high (0.90).
The Freiburg Mindfulness Inventory ( Walach et al., 2006) is a 14-item scale. Many studies validated this scale (e.g. Şakiroğlu et al., 2017; Fathalla, 2018; Elkady, 2019a; Arıcı Özcan, 2021). Cronbach’s alpha was 0.89. The scale correlated positively and significantly with that of Al Behera et al. (2014; r = 0.57, P < 0.01).
The Multidimensional Scale of PSS ( Zimet et al., 1988, translated into Arabic by Elkady, 2019b) consisted of 12 items for three subscales: family, friends, and significant others. Cronbach’s alpha (α) values were 0.78 and 0.82, and 0.91 for the total scale. The scale correlated positively and significantly with that of Kamel (2018; r = 0.43).
Quality of Life Survey ( Maleki et al., 2014) was measured using F-36, which consists of eight subscales. The eight subscales’ Cronbach’s alpha (α) was between 0.79 and 0.89.
Data collection procedure
After visiting the target schools, the researchers were allowed to administer the scales during classes. Participants signed the consent form and returned it. The study was conducted between December 2021 and March 2022.
Data analyses
Data screening procedures for normality were examined using the Kolmogorov–Smirnov test. In the descriptive analysis, calculations were done by using mean and standard deviation (SD). Bivariate correlations were used for calculating correlation. Chi-square value (χ 2), χ 2/df, root mean square error of approximation (RMSEA), comparative fit index (CFI), tucker-lewis index (TLI), and goodness of fit index (GFI) were used to test the goodness of fit of the proposed model. Path analysis through AMOS 18 (IBM ® SPSS ® Amos Version 18) software was used.
RESULTS
In this section, the authors present the results of descriptive statistics of means and SDs for each variable. Intercorrelations among the exogenous PMS variable, PSS mediator variables, and HRQoL and endogenous variable of mindfulness were examined through Pearson product–moment correlation coefficients. The standardized path coefficients for each path were presented.
Descriptive statistics
Descriptive statistics of means and SDs for each variable were computed. Table 1 shows the results for means and SD for variables. As shown in Table 1, the mean score for PMS was 90.27, with an SD of 3.3. The standard for mindfulness was found to be 58.01, with an SD of 4.6, for PSS was 52.21 with an SD of 5.2, and for HRQoL was 69.25 with an SD of 5.7.
Correlations
Intercorrelations among the exogenous PMS variable, PSS mediator variables, and HRQoL and endogenous variable of mindfulness were examined through Pearson product–moment correlation coefficients. The results of correlation analyses are presented in Table 2. As shown in Table 2, bivariate correlations between PSM, PSS, and HRQoL were presented. There was a significant correlation between PMS, mindfulness( r = −0.46, P < 0.001), PSS ( r = −0.49, P < 0.001), and HRQoL ( r = −0.45, P < 0.001). There was a significant positive correlation between mindfulness, PSS ( r = 0.53, P < 0.001), and HRQoL ( r = 0.48, P < 0.001). There was a negative relationship between PSS and HRQoL ( r = 0.47, P < 0.001).
Path analysis for mindfulness model
χ 2, χ 2/df, RMSEA, CFI, TLI, and GFI are indicators of healthy goodness. Table 3 presents acceptable ranges for model fit indices. As shown in Table 3, the Chi-square value was not significant χ 2(1) = (2.4), P = (0.19). This indicates that the model is a good fit. RMSEA value was found to be 0.05. CFI has a value of 1.00, and TLI has a value of 0.99. GFI was calculated to be 1.00.
Model fit indices.
| Goodness of fit | Model fit indices |
|---|---|
| χ 2/df | 2.4; 1 |
| χ 2/df | 2.6 |
| CFI | 1.00 |
| TLI | 0.99 |
| RMSEA | 0.05 |
| GFI | 1.00 |
Figure 2 presents the standardized path coefficients for each path. As shown, PMS has direct effects on PSS (β = −0.45) and HRQoL (β = −0.47). In addition, both PSS (β = −0.33) and HRQoL (β = 0.35) have direct effects on mindfulness. All the paths were found to be significant.
Relationships
Table 4 presents the standardized total, direct, and indirect estimates. They were all significant ( P < 0.001)
Standardized total, direct, and indirect estimates of the proposed model.
| Paths | Standardized estimates (β) |
|---|---|
 | |
| Indirect (total) | −0.38** |
| Indirect by PSS | −0.29** |
| Indirect by HRQoL | −0.27** |
| Indirect by PSS and HRQoL | −0.24** |
 | |
| Direct | 0.36** |
 | |
| Direct | 0.39** |
Abbreviations: HRQoL, health-related quality of life; PSS, perceived social support. ** P < 0.001
DISCUSSION
The aim of this study is to explore the correlation between PMS and mindfulness and the mediating role of PSS and HRQoL among deaf/hard-of-hearing women. Moreover, we examined the direct relationship of PSS and HRQoL to mindfulness.
In the literature, researchers examined the effect of PMS on QoL. For example, Dean et al. (2006) reported that PMS was associated with a significant decrease in QoL. Nour et al. (2009) said that PMS is associated negatively with HRQoL. Zaka and Mahmood (2012) reported that PMS might affect women’s QoL. Moderate to severe premenstrual symptoms adversely affect women and lead to reduced quality of life ( Kahyaoglu Sut and Mestogullari, 2015).
Women with PMS are impaired in physical functioning and psychological health. This may lead to significantly lower QoL ( Malhotra et al., 2020). This means that “girls with menstruation problems have mental health problems and are poor in QoL compared to those without these problems” ( Sarwar and Rauf, 2021, p. 206). Females with menstrual disorders had poorer QoL than those without menstrual disorders ( Laksham et al., 2019). Farrokh-Eslamlou et al. (2015) found that mental health decreases as the PMS increases.
Mindfulness is a strategy that can be useful in decreasing the stress and pressures of daily life. However, it can significantly influence and be useful in healthcare issues, such as PMS. In this case, the forces are great ( Anwaar et al., 2018). Mindfulness application can affect the mind, the autonomic nervous system, stress hormones, the immune system, and physical conditions in helpful ways ( Anwaar et al., 2018).
As indicated by Lustyk et al. (2011), the woman who gets a high score in mindfulness also gets low scores in premenstrual symptom reports. The results of Lustyk et al. (2011) introduce evidence that mindfulness has a positive impact on the severity of premenstrual symptoms. This finding is consistent with what has been reported in the psychological literature. Empirical observations support that mindfulness reduces feelings of suffering and increases positive qualities such as well-being, insight, wisdom, openness, and compassion ( Baer et al., 2012; Bluth and Blanton, 2013; Khaleghi et al., 2019).
It also reduces chronic pain rates, improves body immunity, and reduces anxiety and mood disorders. Mindfulness also facilitates cognitive, affective, and behavioral flexibility and allows for more consensual responses to threatening or challenging situations rather than responding habitually or hastily. In theory, we find that mindfulness facilitates harmonious emotional regulation, which reduces psychological disturbances and stresses and increases the effectiveness of interpersonal relationships ( Pepping et al., 2014).
CONCLUSION
The biological nature of a woman determines the need to pass through certain physiological stages. These stages are linked to psychological changes whose intensity varies from one female to another and in the female herself from time to time. Although these physiological stages are initially subject to biological decisions, they are sometimes affected by social factors or exceptional circumstances. All these stages can be considered periods of stress and exhaustion in the female’s life, and one of these stages is menstruation.
This study examined and confirmed the relationship between PMS and mindfulness as mediated by PSS and HRQoL among deaf/hard-of-hearing women. As indicated by the results, PMS correlated significantly with mindfulness, PSS, and HRQoL. Moreover, mindfulness correlated significantly and positively with PSS and HRQoL. Besides, there is a significant negative relationship between PSS and HRQoL. PMS has direct effects on PSS and HRQoL. In addition, both PSS and HRQoL have immediate impacts on mindfulness. Through mindfulness, the person becomes fully aware of stressful situations.
STRENGTHS AND LIMITATIONS
This study adds to the literature on PMS and mindfulness as mediated by PSS and HRQoL among deaf/hard-of-hearing women. It is the first to investigate the mediating role of PSS and HRQoL on the relationships between PS and mindfulness among deaf/hard-of-hearing women.
However, there are some limitations. First, causal mediation cannot be inferred from cross-sectional design data. Second, girl participants were from Tabuk. This prevents the generalization of findings to more diverse populations. Third, self-report measures may be biased.