- Record: found
- Abstract: found
- Article: found
The Obesity Paradox in Kidney Disease: How to Reconcile It With Obesity Management
Read this article at
Abstract
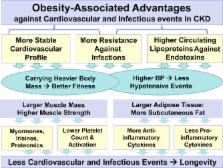
Obesity, a risk factor for de novo chronic kidney disease (CKD), confers survival advantages in advanced CKD. This so-called obesity paradox is the archetype of the reverse epidemiology of cardiovascular risks, in addition to the lipid, blood pressure, adiponectin, homocysteine, and uric acid paradoxes. These paradoxical phenomena are in sharp contradistinction to the known epidemiology of cardiovascular risks in the general population. In addition to advanced CKD, the obesity paradox has also been observed in heart failure, chronic obstructive lung disease, liver cirrhosis, and metastatic cancer, as well as in elderly individuals. These are populations in whom protein−energy wasting and inflammation are strong predictors of early death. Both larger muscle mass and higher body fat provide longevity in these patients, whereas thinner body habitus and weight loss are associated with higher mortality. Muscle mass appears to be superior to body fat in conferring an even greater survival. The obesity paradox may be the result of a time discrepancy between competing risk factors, that is, overnutrition as the long-term killer versus undernutrition as the short-term killer. Hemodynamic stability of obesity, lipoprotein defense against circulating endotoxins, protective cytokine profiles, toxin sequestration of fat mass, and antioxidation of muscle may play important roles. Despite claims that the obesity paradox is a statistical fallacy and a result of residual confounding, the consistency of data and other causality clues suggest a high biologic plausibility. Examining the causes and consequences of the obesity paradox may help uncover important pathophysiologic mechanisms leading to improved outcomes in patients with CKD.
Related collections
Most cited references75
- Record: found
- Abstract: found
- Article: not found
Rosuvastatin and cardiovascular events in patients undergoing hemodialysis.
- Record: found
- Abstract: found
- Article: not found
Causation and causal inference in epidemiology.
- Record: found
- Abstract: found
- Article: not found