- Record: found
- Abstract: found
- Article: found
Adaptive Auricular Point Acupressure for Sleep Disturbance in Women with Breast Cancer: A Randomized Controlled Trial
Read this article at
Abstract
Objectives
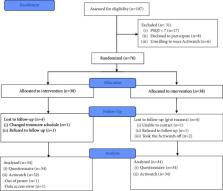
The study aimed to evaluate the preliminary effect and efficacy of auricular point acupressure (APA) on the quality of sleep in women with breast cancer who were undergoing chemotherapy. Sample & Setting. We conducted a randomized controlled trial on 68 patients with breast cancer who reported poor sleep quality based on the Pittsburgh Sleep Quality Index (PSQI) scores (>7). Methods & Variables. Participants were randomly assigned to an APA treatment group or a control group. Patients in the APA group had magnetic pellets attached to selected auricular points and were instructed to apply pressure to these points 4×/day for three consecutive weeks. We objectively measured sleep quality using the Actiwatch Spectrum and the PSQI at the baseline and postintervention. Statistical analyses of changes in sleep data were performed using the t-test, a rank-sum test, and analyses of covariance.
Results
In patients treated with APA, the PSQI total score and sleep onset latency had significantly decreased, while the total sleep time and sleep efficiency had significantly increased. Although the total PSQI score differed between groups at the baseline, ANCOVA results showed that the APA group had a significantly lower total PSQI score.
Related collections
Most cited references54
- Record: found
- Abstract: found
- Article: not found
The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research
- Record: found
- Abstract: found
- Article: not found
Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians.
- Record: found
- Abstract: found
- Article: not found