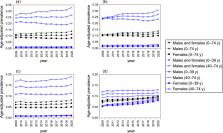
Background: On 11 March 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) to be a global pandemic (1). To curb the spread of the disease, various regional and national governments advocated for social distancing measures with varying degrees of enforcement, ranging from unenforced recommendations to quarantine and business closures. Physical activity is an important determinant of health (2) and is likely affected by social distancing measures. Daily step count, a proxy for physical activity, has been associated with all-cause mortality (3). Beyond physical activity, regional step count trends may also provide a proxy for adherence to social distancing, providing real-time insights to inform public policy decisions. Because prolonged social distancing is considered to contain infection, it will be important to gauge adherence to these measures and their effect on other aspects of health, such as physical activity. Objective: To examine worldwide changes in step count before and after the announcement of COVID-19 as a global pandemic. Methods and Findings: In this descriptive study, we used deidentified, individual-level data from 19 January to 1 June 2020 that were collected from a convenience sample of users of the free, popular health and wellness smartphone app Argus (Azumio). Daily step counts were determined using smartphone accelerometers and Apple or Android algorithms for step counting (4). User location was determined by smartphone IP address. The COVID-19 pandemic declaration date used was 11 March 2020. Regional mean steps were calculated daily, and percentage of change in steps was calculated daily as a percentage of the regional mean from 19 January to 11 March 2020. Displayed figure regions were selected to achieve half less-affected and half more-affected regions with regard to both COVID-19 and social distancing and greater than 1000 and 700 users at the country and city levels, respectively. This study was exempted by the University of California, San Francisco Institutional Review Board. A total of 19 144 639 daily step count measurements were provided by 455 404 unique users from 187 unique countries during the study period; 92% of smartphones were Apple, and 8% were Android. Worldwide, within 10 days of the pandemic declaration, there was a 5.5% decrease in mean steps (287 steps), and within 30 days, there was a 27.3% decrease in mean steps (1432 steps). There was wide regional variation in average step count change and in the timing and rate of that change (Figures 1 and 2). For example, Italy declared a nationwide lockdown on 9 March 2020 and exhibited a 48.7% maximal decrease, whereas Sweden, to date, has primarily advocated for social distancing and limitations on gatherings and showed a 6.9% maximal decrease. Samples from countries such as Italy and Iran, which had earlier regional COVID-19 outbreaks, exhibited earlier step count decreases from their relative baselines. Samples from different countries varied widely in the number of days after pandemic declaration that a 15% step count decrease was seen: Italy (5 days), Spain (9 days), France (12 days), India (14 days), the United States (15 days), the United Kingdom (17 days), Australia (19 days), and Japan (24 days). Step count trends in samples from U.S. cities exhibited similarities, although there was wide international variability (Figure 2). Figure 1. Mean daily steps and percentage of change from step count at baseline by country. Top. Mean daily steps by country. Bottom. Percentage of change in steps from the prepandemic baseline by country. * Prepandemic baseline steps by country were calculated as the mean daily steps from 19 January to 11 March 2020 for that country. All values are plotted by region over a rolling 10-d average window for smoothness. Region sample sizes show total number of users who contributed data during the study period. Diamonds denote initiation dates and squares denote lifting dates of regional social distancing orders, if available. Specific regional orders were assembled from publicly available sources as accurately as possible. Brazil, South Korea, Sweden, Taiwan, and the United States: no national orders. France: stay-at-home orders, only essential businesses open (17 March to 10 May 2020). Iran: lockdown orders, only essential businesses open (14 March to 20 April 2020). Italy: lockdown orders, only essential businesses open (9 March to 18 May 2020). Japan: state of emergency for all prefectures and nonmandatory business closure request (16 April to 25 May 2020). United Kingdom: ongoing stay-at-home orders, only essential businesses open (23 March 2020 to present). Figure 1. Mean daily steps and percentage of change from step count at baseline by country. Top. Mean daily steps by country. Bottom. Percentage of change in steps from the prepandemic baseline by country. * Prepandemic baseline steps by country were calculated as the mean daily steps from 19 January to 11 March 2020 for that country. All values are plotted by region over a rolling 10-d average window for smoothness. Region sample sizes show total number of users who contributed data during the study period. Diamonds denote initiation dates and squares denote lifting dates of regional social distancing orders, if available. Specific regional orders were assembled from publicly available sources as accurately as possible. Brazil, South Korea, Sweden, Taiwan, and the United States: no national orders. France: stay-at-home orders, only essential businesses open (17 March to 10 May 2020). Iran: lockdown orders, only essential businesses open (14 March to 20 April 2020). Italy: lockdown orders, only essential businesses open (9 March to 18 May 2020). Japan: state of emergency for all prefectures and nonmandatory business closure request (16 April to 25 May 2020). United Kingdom: ongoing stay-at-home orders, only essential businesses open (23 March 2020 to present). Figure 2. Mean daily steps and percentage of change from step count at baseline by city. A. Mean daily steps by U.S. city. B. Percentage of change in steps from the prepandemic baseline by U.S. city. C. Mean daily steps in a sample of cities worldwide. D. Percentage of change in steps from the prepandemic baseline in a sample of cities worldwide. * Prepandemic baseline steps by city were calculated as the mean daily steps from 19 January to 11 March 2020 for that city. All values are plotted by region over a rolling 10-d average window for smoothness. Region sample sizes show the total number of users who contributed data during the study period. Diamonds denote initiation dates and squares denote lifting dates of regional social distancing orders, if available. Specific regional orders were assembled from publicly available sources as accurately as possible. Chicago: stay-at-home order, only essential businesses open (21 March to 3 June 2020). Dallas: shelter-in-place order, only essential businesses open (24 March to 30 April 2020). Houston: stay-at-home order, only essential businesses open (24 March to 30 April 2020). Los Angeles: ongoing stay-at-home order, only essential businesses open (19 March 2020 to present). New York City: ongoing shelter-in-place order, only essential businesses open (22 March 2020 to present). Philadelphia: stay-at-home order, only essential businesses open (23 March to 5 June 2020). Phoenix: stay-at-home order, phased reopening (31 March to 15 May 2020). San Antonio: stay-at-home order, only essential businesses open (24 March to 30 April 2020). San Diego: ongoing stay-at-home order, only essential businesses open (19 March 2020 to present). San Jose: ongoing stay-at-home order, only essential businesses open (17 March 2020 to present). Ho Chi Minh City: nationwide isolation, only essential activities allowed (1 April to 22 April 2020). London: ongoing stay-at-home orders, only essential businesses open (23 March 2020 to present). New York City: ongoing shelter-in-place order, only essential businesses open (22 March 2020 to present). Paris: stay-at-home order, only essential businesses open (17 March to 10 May 2020). Rome: lockdown orders, only essential businesses open (9 March to 17 May 2020). Sao Paulo: ongoing statewide quarantine, only essential businesses open (24 March 2020 to present). Seoul: no regional orders, citizens asked to remain indoors for 2 weeks starting 29 February 2020. Singapore: stay-at-home order, limits on social gatherings (7 April to 1 June 2020). Stockholm: no regional orders. Tokyo: state of emergency for Tokyo, nonmandatory business closure request (7 April to 25 May 2020). Figure 2. Mean daily steps and percentage of change from step count at baseline by city. A. Mean daily steps by U.S. city. B. Percentage of change in steps from the prepandemic baseline by U.S. city. C. Mean daily steps in a sample of cities worldwide. D. Percentage of change in steps from the prepandemic baseline in a sample of cities worldwide. * Prepandemic baseline steps by city were calculated as the mean daily steps from 19 January to 11 March 2020 for that city. All values are plotted by region over a rolling 10-d average window for smoothness. Region sample sizes show the total number of users who contributed data during the study period. Diamonds denote initiation dates and squares denote lifting dates of regional social distancing orders, if available. Specific regional orders were assembled from publicly available sources as accurately as possible. Chicago: stay-at-home order, only essential businesses open (21 March to 3 June 2020). Dallas: shelter-in-place order, only essential businesses open (24 March to 30 April 2020). Houston: stay-at-home order, only essential businesses open (24 March to 30 April 2020). Los Angeles: ongoing stay-at-home order, only essential businesses open (19 March 2020 to present). New York City: ongoing shelter-in-place order, only essential businesses open (22 March 2020 to present). Philadelphia: stay-at-home order, only essential businesses open (23 March to 5 June 2020). Phoenix: stay-at-home order, phased reopening (31 March to 15 May 2020). San Antonio: stay-at-home order, only essential businesses open (24 March to 30 April 2020). San Diego: ongoing stay-at-home order, only essential businesses open (19 March 2020 to present). San Jose: ongoing stay-at-home order, only essential businesses open (17 March 2020 to present). Ho Chi Minh City: nationwide isolation, only essential activities allowed (1 April to 22 April 2020). London: ongoing stay-at-home orders, only essential businesses open (23 March 2020 to present). New York City: ongoing shelter-in-place order, only essential businesses open (22 March 2020 to present). Paris: stay-at-home order, only essential businesses open (17 March to 10 May 2020). Rome: lockdown orders, only essential businesses open (9 March to 17 May 2020). Sao Paulo: ongoing statewide quarantine, only essential businesses open (24 March 2020 to present). Seoul: no regional orders, citizens asked to remain indoors for 2 weeks starting 29 February 2020. Singapore: stay-at-home order, limits on social gatherings (7 April to 1 June 2020). Stockholm: no regional orders. Tokyo: state of emergency for Tokyo, nonmandatory business closure request (7 April to 25 May 2020). Discussion: Step counts decreased worldwide in the period after COVID-19 was declared a global pandemic. Differences were seen between regions, likely reflecting regional variation in COVID-19 timing, regional enforcement, and behavior change. Countries that, to date, have had relatively low COVID-19 infection rates and have therefore not instituted lockdowns, such as South Korea, Taiwan, and Japan, have still exhibited decreases in overall step count. Within-region step count trends likely reflect a combination of changes to physical activity (for example, walking and exercising) and activities of daily living (for example, commuting and shopping) due to social distancing efforts. Assuming no regulatory changes that affect engaging in physical activity within a region, we suspect that sustained population-level trends over time may reflect changes to social distancing adherence (for example, many regions showed increases from their regional step count nadir before orders were lifted). Observed variation in step counts is also likely influenced by socioeconomic inequalities among regions and disparities in the ability to engage in or access to recreational physical activity within a region (4). Limitations of this study include sampling bias due to the reliance on smartphone and app ownership, measurement error from smartphone-measured step counts, variability in smartphone carry and use habits, no assessment of activity intensity, and inability to capture nonstepping exercise (5). Our data set is a nonrepresentative convenience sample with a variable number of contributing daily users. It also lacks participant characteristics beyond IP address, limiting comparisons among regions. Rapid worldwide step count decreases have been seen during the COVID-19 pandemic, with regional variability. Within-region step count trends may reflect social distancing measures and changes to social distancing adherence; however, more formal analytic studies are required. The effect of social distancing measures on overall physical activity, an important determinant of health, should be considered, particularly if prolonged social distancing is required.