- Record: found
- Abstract: found
- Article: found
Preventing venous thromboembolism in oncology practice: Use of risk assessment and anticoagulation prophylaxis
Read this article at
Abstract
Background
Venous thromboembolism (VTE) is a leading cause of morbidity and mortality in patients with cancer. Expert consensus recommends a risk‐based approach to guide prophylactic anticoagulation to prevent VTE in ambulatory patients with cancer receiving chemotherapy. However, oncology practice patterns for VTE prevention remain unclear.
Patients/Methods
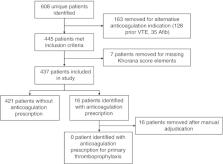
We conducted (i) a retrospective, single‐center cohort study of patients with pancreatic and gastric cancers to examine rates of prophylactic anticoagulation prescription for eligible patients at high risk of VTE based on the validated Khorana score, and (ii) a 15‐question survey of oncology clinicians at the same institution to assess current practice patterns and knowledge regarding VTE risk assessment and primary thromboprophylaxis in February 2020.
Results
Of 437 patients who met study criteria, 181 (41%) had a score of ≥ 3 (high‐risk), and none had an anticoagulation prescription for prophylaxis without an alternate treatment indication. In a survey sent to 98 oncology clinicians, of which 34 participated, 67% were unfamiliar with the Khorana score or guideline recommendations regarding risk‐based VTE prophylaxis, and 90% “never” or “rarely” used VTE risk assessment.
Related collections
Most cited references12
- Record: found
- Abstract: found
- Article: not found
Epidemiology of cancer-associated venous thrombosis.
- Record: found
- Abstract: found
- Article: not found
Development and validation of a predictive model for chemotherapy-associated thrombosis.
- Record: found
- Abstract: not found
- Article: not found