- Record: found
- Abstract: found
- Article: found
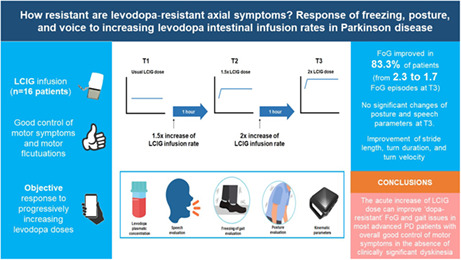
How resistant are levodopa‐resistant axial symptoms? Response of freezing, posture, and voice to increasing levodopa intestinal infusion rates in Parkinson disease

Read this article at
Abstract
Background and purpose
Treatment of freezing of gait (FoG) and other Parkinson disease (PD) axial symptoms is challenging. Systematic assessments of axial symptoms at progressively increasing levodopa doses are lacking. We sought to analyze the resistance to high levodopa doses of FoG, posture, speech, and altered gait features presenting in daily‐ON therapeutic condition.
Methods
We performed a pre‐/postinterventional study including patients treated with levodopa/carbidopa intestinal gel infusion (LCIG) with disabling FoG in daily‐ON condition. Patients were evaluated at their usual LCIG infusion rate (T1), and 1 h after 1.5× (T2) and 2× (T3) increase of the LCIG infusion rate by quantitative outcome measures. The number of FoG episodes (primary outcome), posture, speech, and gait features were objectively quantified during a standardized test by a blinded rater. Changes in motor symptoms, dyskinesia, and plasma levodopa concentrations were also analyzed.
Results
We evaluated 16 patients with a mean age of 69 ± 9.4 years and treated with LCIG for a mean of 2.2 ± 2.1 years. FoG improved in 83.3% of patients by increasing the levodopa doses. The number of FoG episodes significantly decreased (mean = 2.3 at T1, 1.7 at T2, 1.2 at T3; p = 0.013). Posture and speech features did not show significant changes, whereas stride length ( p = 0.049), turn duration ( p = 0.001), and turn velocity ( p = 0.024) significantly improved on doubling the levodopa infusion rate.
Abstract
Related collections
Most cited references46
- Record: found
- Abstract: found
- Article: not found
MDS clinical diagnostic criteria for Parkinson's disease.
- Record: found
- Abstract: found
- Article: not found