- Record: found
- Abstract: found
- Article: found
Effect of body mass index on pregnancy outcomes in a freeze-all policy: an analysis of 22,043 first autologous frozen-thawed embryo transfer cycles in China
Read this article at
Abstract
Background
Abnormal BMI is associated with discouraging IVF outcomes in fresh autologous or oocyte donor cycles, whether or not such a relation also holds true for women undergoing frozen-thawed embryo transfer (FET) remains unknown. In addition, it remains unclear the detrimental effect of abnormal BMI on IVF outcomes occurs at the level of ovary or endometrium.
Methods
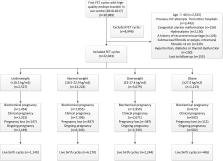
A retrospective study involved 22,043 first FET cycles of all women who had undergone a freeze-all policy during the period from January 2010 to June 2017. To control for the embryo factor, our analysis was restricted to women with high-quality embryo transfer. The main outcome measure was live birth rate per embryo transfer. The secondary endpoints included rates of implantation, clinical pregnancy, multiple pregnancy, and pregnancy loss. Multivariate logistic regression analysis was performed to detect the independent effect of BMI on live birth rate after adjusting for important confounding variables.
Results
In the crude analysis, reproductive outcomes were similar between underweight women and normal-weight controls whereas all parameter outcomes were significantly worse in patients with obesity. After adjustment for a number of confounding factors, underweight women had a marginally significant decrease in rates of implantation (adjusted odds ratio (aOR) 0.91; 95% CI 0.85–0.96), clinical pregnancy (aOR 0.91; 95% CI 0.83–0.99), and live birth (aOR 0.91; 95% CI 0.83–0.99) as compared to the women with normal weight. Obesity was significantly associated with decreased implantation (aOR 0.80; 95% CI 0.73–0.87), clinical pregnancy (aOR 0.81; 95% CI 0.71–0.91), and live birth rates (aOR 0.70; 95% CI 0.62–0.80). Moreover, the pregnancy loss rate, both in the first (aOR 1.46; 95% CI 1.15–1.87) and in the second trimester (aOR 2.76; 95% CI 1.67–4.58), was significantly higher in the obesity group than that in the reference group.
Conclusions
Among women undergoing first FET with high-quality embryo transfer, low BMI has limited impact on pregnancy and live birth rates. On the contrary, obesity was associated with worse IVF outcomes. Our findings further highlighted that endometrial receptivity played an important role in the poor reproductive outcomes of women with abnormal weight status.
Related collections
Most cited references27
- Record: found
- Abstract: not found
- Article: not found
International Committee for Monitoring Assisted Reproductive Technology: world report on assisted reproductive technology, 2011
- Record: found
- Abstract: found
- Article: not found
Obesity affects spontaneous pregnancy chances in subfertile, ovulatory women.
- Record: found
- Abstract: found
- Article: not found