- Record: found
- Abstract: found
- Article: found
Type distribution of human papillomavirus among adult women diagnosed with invasive cervical cancer (stage 1b or higher) in New Zealand
Read this article at
Abstract
Background
Human papillomavirus (HPV) is the necessary cause of cervical cancer. Published data on the epidemiology of HPV in women with invasive cervical cancer (ICC) in New Zealand (NZ) are limited. This cross-sectional study investigated the distribution of high-risk and low-risk HPV types in cervical specimens collected from women throughout NZ who had been diagnosed with ICC between 2004 and 2010.
Methods
Women aged ≥18 years, with ICC International Federation of Gynecology and Obstetrics stage Ib or greater were identified from the five tertiary public hospitals in NZ regularly treating women with ICC. Women were enrolled in the study only after obtaining informed consent. Stored, formalin fixed, paraffin-embedded cervical specimens were retrieved and histopathologically reviewed to confirm the diagnosis of ICC. Cervical specimens were tested for HPV using polymerase chain reaction-short fragment10; HPV DNA was detected using DNA enzyme immunoassay and typed by reverse hybridization line probe assay.
Results
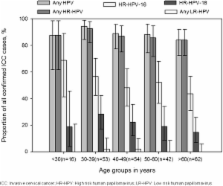
242 women were enrolled and ICC was histologically confirmed in 227 samples. HPV infection was detected in 88.5% (n = 201; 95% CI: 83.7–92.4) of women with ICC; high-risk HPV types were detected in 87.2% of women. The most commonly detected HPV types were HPV-16 (51.1%) and HPV-18 (20.7%), followed by HPV-31 (4.0%), HPV-45 and HPV-52 (3.1% each). Overall, HPV distribution was highest (94.3%) in women aged 30–39 years at diagnosis and a higher distribution of HPV-16 (68.8%) was observed in women younger than 30 years. The overall distribution of HPV types between Maori and non-Maori women were similar. HPV-positive women with ICC stage II or greater were less likely to be infected with HPV-16/18 ( P = 0.002) or HPV-18 ( P = 0.029) compared with the other high-risk types. Single type infection and multiple infections were detected in 93.5% and 5.5% of women, respectively.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update.
- Record: found
- Abstract: found
- Article: not found
Worldwide burden of cervical cancer in 2008.
- Record: found
- Abstract: found
- Article: not found