- Record: found
- Abstract: found
- Article: found
A prospective multicentre study testing the diagnostic accuracy of an automated cough sound centred analytic system for the identification of common respiratory disorders in children
Read this article at
Abstract
Background
The differential diagnosis of paediatric respiratory conditions is difficult and suboptimal. Existing diagnostic algorithms are associated with significant error rates, resulting in misdiagnoses, inappropriate use of antibiotics and unacceptable morbidity and mortality. Recent advances in acoustic engineering and artificial intelligence have shown promise in the identification of respiratory conditions based on sound analysis, reducing dependence on diagnostic support services and clinical expertise. We present the results of a diagnostic accuracy study for paediatric respiratory disease using an automated cough-sound analyser.
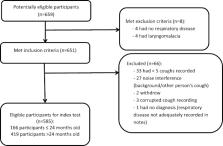
Methods
We recorded cough sounds in typical clinical environments and the first five coughs were used in analyses. Analyses were performed using cough data and up to five-symptom input derived from patient/parent-reported history. Comparison was made between the automated cough analyser diagnoses and consensus clinical diagnoses reached by a panel of paediatricians after review of hospital charts and all available investigations.
Results
A total of 585 subjects aged 29 days to 12 years were included for analysis. The Positive Percent and Negative Percent Agreement values between the automated analyser and the clinical reference were as follows: asthma (97, 91%); pneumonia (87, 85%); lower respiratory tract disease (83, 82%); croup (85, 82%); bronchiolitis (84, 81%). Conclusion: The results indicate that this technology has a role as a high-level diagnostic aid in the assessment of common childhood respiratory disorders.
Trial registration
Australian and New Zealand Clinical Trial Registry (retrospective) - ACTRN12618001521213: 11.09.2018.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis.
- Record: found
- Abstract: found
- Article: not found