- Record: found
- Abstract: found
- Article: found
Mental disorders in Bangladesh: a systematic review
Read this article at
Abstract
Background
Mental disorders constitute a major public health problem globally with higher burden in low and middle-income countries. In Bangladesh, systematically-collected data on mental disorders are scarce and this leaves the extent of the problem not so well defined. We reviewed the literature on mental health disorders in Bangladesh to summarize the available data and identify evidence gaps.
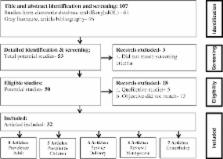
Methods
We identified relevant literature on mental disorders within Bangladesh published between 1975 and October, 2013 through a systematic and comprehensive search. Relevant information from the selected articles was extracted and presented in tables.
Results
We identified 32 articles which met our pre-defined eligibility criteria. The reported prevalence of mental disorders varied from 6.5 to 31.0% among adults and from 13.4 to 22.9% among children. Some awareness regarding mental health disorders exists at community level. There is a negative attitude towards treatment of those affected and treatment is not a priority in health care delivery. Mental health services are concentrated around tertiary care hospitals in big cities and absent in primary care.
Related collections
Most cited references62
- Record: found
- Abstract: found
- Article: not found
The prevalence of comorbid depression in adults with diabetes: a meta-analysis.
- Record: found
- Abstract: found
- Article: not found
Depression and poor glycemic control: a meta-analytic review of the literature.
- Record: found
- Abstract: found
- Article: not found