- Record: found
- Abstract: found
- Article: found
Vascular Occlusions following Ocular Surgical Procedures: A Clinical Observation of Vascular Complications after Ocular Surgery
Read this article at
Abstract
Background
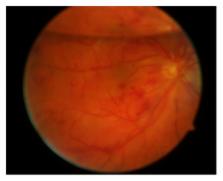
Ocular vascular occlusions following intraocular procedures are a rare complication. We report a case series of patients with retinal vascular occlusions or anterior ischemic optic neuropathy (AION) after anterior and posterior segment surgery and demonstrate possible risk factors.
Results
In ten patients, vascular occlusions were observed within ten weeks after intraocular surgery: branch retinal arterial occlusion (BRAO) ( n = 2), central retinal artery occlusion (CRAO) ( n = 2), central retinal vein occlusion (CRVO) ( n = 1), branch retinal vein occlusion (BRVO) ( n = 1), anterior ischemic optic neuropathy (AION) ( n = 3), and combined central artery and vein occlusion ( n = 1). AION occurred later (27–69 d) than arterial occlusions (14–60 d) or venous occlusions (1-2 d). In all cases, either specific surgical manipulations or general vascular disorders were identified as risk factors. In addition to general cardiovascular risk factors (arterial hypertension n = 6, diabetes mellitus n = 4), internal workup disclosed bilateral stenosis of the carotid arteries ( n = 1) and myeloproliferative syndrome ( n = 1).
Conclusion
Vascular occlusions after surgical ocular procedures seem to be more frequent when cardiovascular diseases coexist. Surgical maneuvers and intra- or postoperative pressure changes may act as a triggering mechanism in patients with underlying systemic cardiovascular disorders. Affected patients should undergo thorough internal examination to identify possible underlying diseases.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Risk factors for central retinal vein occlusion. The Eye Disease Case-Control Study Group.
- Record: found
- Abstract: found
- Article: not found
Management of glaucoma after retinal detachment surgery.
- Record: found
- Abstract: found
- Article: not found