- Record: found
- Abstract: found
- Article: found
Local delivery of EGFR +NSCs-derived exosomes promotes neural regeneration post spinal cord injury via miR-34a-5p/HDAC6 pathway

Read this article at
Abstract
Spinal cord injury (SCI) causes severe axon damage, usually leading to permanent paraparesis, which still lacks effective regenerative therapy. Recent studies have suggested that exosomes derived from neural stem cells (NSCs) may hold promise as attractive candidates for SCI treatment. Epidermal Growth Factor Receptor positive NSC (EGFR +NSC) is a subpopulation of endogenous NSCs, showing strong regenerative capability in central nervous system disease. In the current study, we isolated exosomes from the EGFR +NSCs (EGFR +NSCs-Exos) and discovered that local delivery of EGFR +NSCs-Exos can effectively promote neurite regrowth in the injury site of spinal cord-injured mice and improve their neurological function recovery. Using the miRNA-seq, we firstly characterized the microRNAs (miRNAs) cargo of EGFR +NSCs-Exos and identified miR-34a-5p which was highly enriched in EGFR +NSCs derived exosomes. We further interpreted that exosomal miR-34a-5p could be transferred to neurons and inhibit the HDAC6 expression by directly binding to its mRNA, contributing to microtubule stabilization and autophagy induction for aiding SCI repair. Overall, our research demonstrated a novel therapeutic approach to improving neurological functional recovery by using exosomes secreted from a subpopulation of endogenous NSCs and providing a precise cell-free treatment strategy for SCI repair.
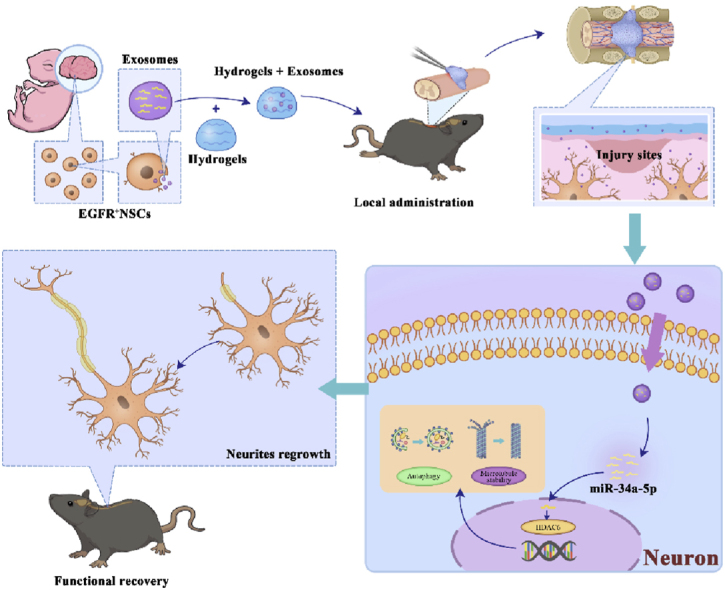
Graphical abstract
In this study, we identified a subtype of NSCs, named EGFR +NSCs, and extracted their exosomes, which were superior in SCI repair. We demonstrated that EGFR +NSCs-derived exosomes could cross the blood-spinal cord barrier (BSCB) and downregulate HDAC6 in neurons by delivering exosomal miR-34a-5p. And the inhibition of HDAC6 activated the autophagy pathway and promoted microtubule stability to facilitate neurite growth. It highlights that EGFR +NSCs-derived exosomes can serve as a novel therapeutic agent for spinal cord injury (SCI) repair.
Highlights
-
•
EGFR +NSCs, as a subpopulation, secrete exosomes with a more potent ability to effectively promote neural regeneration.
-
•
EGFR +NSCs-Exos enhance neural autophagy and microtubule stability via the miR-34a-5p/HDAC6-dependent pathway.
-
•
Local delivery of EGFR +NSCs-Exos using 3D-printed hydrogel patches provides a precise, cell-free treatment strategy for SCI repair.
Related collections
Most cited references65
- Record: found
- Abstract: found
- Article: not found
Traumatic spinal cord injury

- Record: found
- Abstract: found
- Article: found