- Record: found
- Abstract: found
- Article: found
Current status of preoperative risk assessment for posthepatectomy liver failure in patients with hepatocellular carcinoma

Read this article at
Abstract
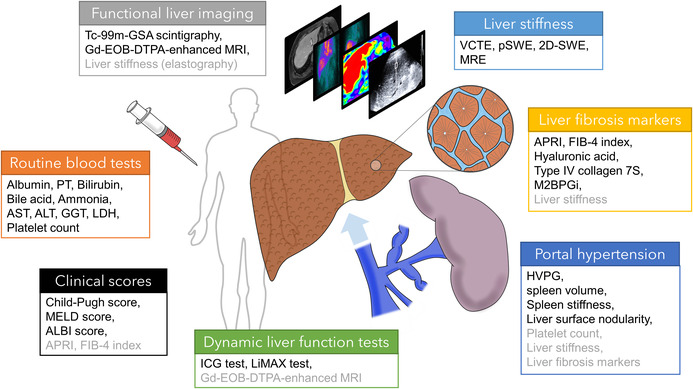
Liver resection is an effective therapeutic option for patients with hepatocellular carcinoma. However, posthepatectomy liver failure (PHLF) remains a major cause of hepatectomy‐related mortality, and the accurate prediction of PHLF based on preoperative assessment of liver functional reserve is a critical issue. The definition of PHLF proposed by the International Study Group for Liver Surgery has gained acceptance as a standard grading criterion. Liver function can be estimated using a variety of parameters, including routine blood biochemical examinations, clinical scoring systems, dynamic liver function tests, liver stiffness and fibrosis markers, and imaging studies. The Child–Pugh score and model for end‐stage liver disease scores are conventionally used for estimating liver decompensation, although the alternatively developed albumin‐bilirubin score shows superior performance for predicting hepatic dysfunction. Indocyanine green clearance, a dynamic liver function test mostly used in Japan and other Asian countries, serves as a quantitative estimation of liver function reserve and helps determine indications for surgical procedures according to the estimated risk of PHLF. In an attempt to improve predictive accuracy, specific evaluation of liver fibrosis and portal hypertension has gained popularity, including liver stiffness measurements using ultrasonography or magnetic resonance elastography, as well as noninvasive fibrosis markers. Imaging modalities, including Tc‐99m‐labeled galactosyl serum albumin scintigraphy and gadolinium‐enhanced magnetic resonance imaging, are used for preoperative evaluation in combination with liver volume. This review aims to provide an overview of the usefulness of current options for the preoperative assessment of liver function in predicting PHLF.
Abstract
Posthepatectomy liver failure remains a major cause of hepatectomy‐related mortality, and the accurate prediction of PHLF based on preoperative assessment of liver functional reserve is a critical issue. Multiple studies have evaluated the predictive performance of various preoperative parameters, which are broadly categorized as clinical scores based on routine blood tests, dynamic liver function tests, liver stiffness and noninvasive fibrosis markers, liver function imaging, and biomarkers for portal hypertension. This review aims to provide an overview of the utility of current options for preoperative assessment of liver function and the performance of each parameter in predicting PHLF.
Related collections
Most cited references186
- Record: found
- Abstract: not found
- Article: not found
EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma
- Record: found
- Abstract: found
- Article: not found
Hepatocellular carcinoma
- Record: found
- Abstract: not found
- Article: not found