- Record: found
- Abstract: found
- Article: found
Value of a combined magnetic resonance imaging-based radiomics-clinical model for predicting extracapsular extension in prostate cancer: a preliminary study
Read this article at
Abstract
Background
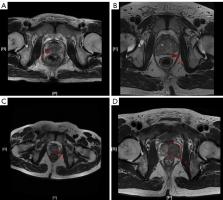
Extracapsular extension (ECE) of prostate cancer (PCa) is closely related to the treatment and prognosis of patients, and radiomics has been widely used in the study of PCa. This study aimed to evaluate the value of a combined model considering magnetic resonance imaging (MRI)-based radiomics and clinical parameters for predicting ECE in PCa.
Methods
A total of 392 PCa patients enrolled in this retrospective study were randomly divided into the training and validation sets at a ratio of 7:3. Radiologists assessed all lesions by Mehralivand grade. Radiomics features were extracted and selected to build a radiomics model, while clinical parameters were noted to construct the clinical model. The combined model was constructed by the integration of the radiomics model and clinical model. Meanwhile, the nomogram for predicting ECE was constructed based on the combined model. Then, the area under the receiver operating characteristic (ROC) curve (AUC), Delong test and the decision curve analysis (DCA) were used to compare the performance among the combined model, radiomics model, clinical model and Mehralivand grade.
Results
The AUC of the combined model in the validation set was comparable to that of the radiomics model [AUC =0.894 (95% confidence interval (CI): 0.837–0.950) vs. 0.835 (95% CI: 0.763–0.908), P>0.05]. In addition, the sensitivity of the combined model and radiomics model was 90.7% and 77.8%, with an accuracy of 81.4% and 76.3%, respectively. On the other hand, the AUCs of the Mehralivand grade of radiologists and clinical model were 0.774 (95% CI: 0.691–0.857) and 0.749 (95% CI: 0.658–0.840), respectively, in the validation set, which were lower than those in the combined model (P<0.05). The DCA implied that the combined model could obtain the maximum net clinical benefits compared with the clinical model, the Mehralivand grade and radiomics model.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Cancer Statistics, 2021
- Record: found
- Abstract: not found
- Article: not found
Regularization Paths for Generalized Linear Models via Coordinate Descent
- Record: found
- Abstract: found
- Article: not found