- Record: found
- Abstract: found
- Article: found
Vaccination against pandemic A/H1N1 2009 influenza in pregnancy and risk of fetal death: cohort study in Denmark
Read this article at
Abstract
Objective To investigate whether an adjuvanted pandemic A/H1N1 2009 influenza vaccine in pregnancy was associated with an increased risk of fetal death.
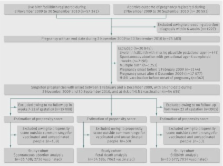
Design Nationwide register based cohort study.
Setting Denmark.
Participants All clinically recognised singleton pregnancies that ended between November 2009 and September 2010. Individual level data on exposure to an inactivated AS03 pandemic A/H1N1 2009 influenza vaccine (Pandemrix) and potential confounders were linked to the study cohort using a unique person identifier.
Main outcome measures The primary outcome measure was risk of fetal death (spontaneous abortion and stillbirth combined) in H1N1 vaccinated compared with unvaccinated pregnancies, adjusting for propensity scores. Secondary outcome measures were spontaneous abortion (between seven and 22 weeks’ gestation) and stillbirth (after 22 completed weeks’ gestation).
Results The cohort comprised 54 585 pregnancies; 7062 (12.9%) women were vaccinated against pandemic A/H1N1 2009 influenza during pregnancy. Overall, 1818 fetal deaths occurred (1678 spontaneous abortions and 140 stillbirths). Exposure to the H1N1 vaccine was not associated with an increased risk of fetal death (adjusted hazard ratio 0.79, 95% confidence interval 0.53 to 1.16), or the secondary outcomes of spontaneous abortion (1.11, 0.71 to 1.73) and stillbirth (0.44, 0.20 to 0.94). Estimates for fetal death were similar in pregnant women with (0.82, 0.44 to 1.53) and without comorbidities (0.77, 0.47 to 1.25).
Conclusion This large cohort study found no evidence of an increased risk of fetal death associated with exposure to an adjuvanted pandemic A/H1N1 2009 influenza vaccine during pregnancy.
Related collections
Most cited references20

- Record: found
- Abstract: found
- Article: found
Long Term Outcomes Following Hospital Admission for Sepsis Using Relative Survival Analysis: A Prospective Cohort Study of 1,092 Patients with 5 Year Follow Up

- Record: found
- Abstract: found
- Article: found
Preparation of Artificial Plasma Membrane Mimicking Vesicles with Lipid Asymmetry

- Record: found
- Abstract: found
- Article: found