- Record: found
- Abstract: found
- Article: found
Inflammatory Myofibroblastic Tumor of the Sciatic Nerve Mimicking Lumbar Disc Herniation: A Diagnostic Challenge
Read this article at
Abstract
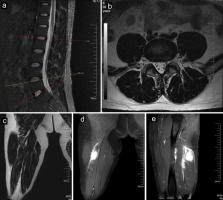
Inflammatory myofibroblastic tumors (IMTs), which involve the proliferation of fibroblastic-myofibroblastic cells mixed with inflammatory infiltrates, are exceedingly rare in the extremities. There are no reported IMTs involving the sciatic nerve. This type of involvement may cause entrapment of the sciatic nerve, whose symptoms may mimic lumbar disc herniation (LDH), especially when it occurs in patients with lumbar degenerative disc disease. We describe the case of a 40-year-old male with lumbar degenerative disc disease accompanied by IMT involving the sciatic nerve whose symptoms mimicked LDH and posed a diagnostic challenge. We showed the course of the disease as well as the systematic imaging manifestations of IMTs involving the sciatic nerve and discussed their therapeutic management.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases.
- Record: found
- Abstract: found
- Article: not found
Targeting ALK With Crizotinib in Pediatric Anaplastic Large Cell Lymphoma and Inflammatory Myofibroblastic Tumor: A Children's Oncology Group Study.
- Record: found
- Abstract: found
- Article: not found