- Record: found
- Abstract: found
- Article: found
Improving outpatient clinic experience: the future of chronic kidney disease care and associated multimorbidity
Read this article at
Abstract
Background
Chronic kidney disease (CKD) is estimated to affect more than 2.5 million adults in England, and this is expected to rise to 4.2 million by 2036 (1). Population-level digital healthcare systems have the potential to enable earlier detection of CKD providing an opportunity to introduce interventions that attenuate progression and reduce the risk of end-stage kidney disease (ESKD) and cardiovascular diseases (CVD). Services that can support patients with CKD, CVD, and diabetes mellitus (DM) have the potential to reduce fragmented clinical care and optimise pharmaceutical management.
Methods and results
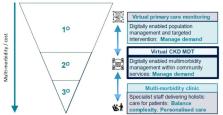
The Salford renal service has established an outpatient improvement programme which aims to address these issues via two projects. Firstly, the development of a CKD dashboard that can stratify patients by their kidney failure risk equation (KFRE) risk. High-risk patients would be invited to attend an outpatient clinic if appropriate. Specialist advice and guidance would be offered to primary care providers looking after patients with medium risk. Patients with lower risk would continue with standard care via their primary care provider unless there was another indication for a nephrology referral. The CKD dashboard identified 11546 patients (4.4% of the total adult population in Salford) with T2DM and CKD. The second project is the establishment of the Metabolic CardioRenal (MRC) clinic. It provided care for 209 patients in the first 8 months of its establishment with a total of 450 patient visits. Initial analysis showed clustering of cardiorenal metabolic diseases with 85% having CKD stages 3 and 4 and 73.2% having DM. In addition, patients had a significant burden of CVD with 50.2% having hypertension and 47.8% having heart failure.
Conclusion
There is a pressing need to create new outpatient models of care to tackle the rising epidemic of cardio-renal metabolic diseases. This model of service has potential benefits at both organisational and patient levels including improving patient management via risk stratification, increased care capacity and reduction of variation of care. Patients will benefit from earlier intervention, appropriate referral for care, reduction in CKD-related complications, and reduction in hospital visits and cardiovascular events. In addition, this combined digital and patient-facing model of care will allow rapid translation of advances in cardio-renal metabolic diseases into clinical practice.
Related collections
Most cited references4

- Record: found
- Abstract: found
- Article: found
The Kidney Failure Risk Equation for prediction of end stage renal disease in UK primary care: An external validation and clinical impact projection cohort study
- Record: found
- Abstract: found
- Article: not found
Novel combined management approaches to patients with diabetes, chronic kidney disease and cardiovascular disease.

- Record: found
- Abstract: found
- Article: found