- Record: found
- Abstract: found
- Article: found
Two-Stage Revision Total Knee Arthroplasty in Cases of Periprosthetic Joint Infection: An Analysis of 50 Cases
Read this article at
Abstract
Objectives: A periprosthetic joint infection (PJI) is a significant complication after total knee arthroplasty (TKA). Still there is no agreement on a perfect diagnosis and treatment algorithm. The aim of this study was to evaluate the success and revision rates after two-stage revision total knee arthroplasty (TKA) and factors that affect the success rate.
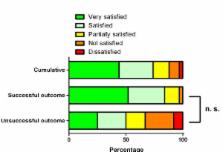
Material and Methods: 50 consecutive two-stage revision TKAs were performed between January 2011 and December 2012. We retrospectively reviewed study patient's charts including demographics, prior surgeries, comorbidities, incidence of persistent infection and revisions. At the final follow-up examination the patient's satisfaction, pain level and disorders were evaluated. A successful clinical outcome was defined as a functioning prosthesis without wound healing disorders, no sinuses tracts or other clinical evidence of a persistent infection.
Results : Re-implantation of prosthesis was performed in 47 cases; three patients received a septic arthrodesis. Twelve patients had a persistent infection despite two-stage re-implantation resulting in a success rate of 76.0%. In eight of these twelve patients an infecting germ was isolated during second-stage procedure. Three patients received another two-stage revision arthroplasty and one patient an above knee amputation. A revision was performed in 23 of 50 patients (46.0%). Factors that diminish the success rate were further operations after primary TKA ( p = 0.048), prior revision arthroplasties after TKA ( p = 0.045), nicotine abuse ( p = 0.048), Charlson comorbidity index above a score of 2 ( p = 0.031) and a mixed flora during first-stage procedure ( p < 0.001). Age, sex, immune status, chronic anticoagulant use, rheumatoid arthritis, body mass index and the presence of multidrug resistant germs showed no significant effect on success rate ( p > 0.05).
Conclusion : We found that patients who required surgery after the primary TKA, had a higher Charlson comorbidity index or were found to have mixed flora during explantation. The treatment of PJI remains difficult, both for the patient and for the treating surgeons.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation
- Record: found
- Abstract: found
- Article: not found
Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found