- Record: found
- Abstract: found
- Article: found
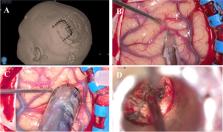
How I do it: parietal trans-sulcal para-fascicular approach to lateral thalamic/internal capsule cavernous malformation
Read this article at
Abstract
Background
The surgical management of deep brain lesions is challenging, with significant morbidity. Advances in surgical technology have presented the opportunity to tackle these lesions.
Methods
We performed a complete resection of a thalamic/internal capsule CM using a tubular retractor system via a parietal trans-sulcal para-fascicular (PTPF) approach without collateral injury to the nearby white matter tracts.
Conclusion
PTPF approach to lateral thalamic/internal capsule lesions can be safely performed without injury to eloquent white matter fibres. The paucity of major vessels along this trajectory and the preservation of lateral ventricle integrity make this approach a feasible alternative to traditional approaches.
Related collections
Most cited references7
- Record: found
- Abstract: found
- Article: not found
Hemorrhage from cerebral cavernous malformations: a systematic pooled analysis.
- Record: found
- Abstract: found
- Article: not found
Cerebral cavernous malformations: natural history and prognosis after clinical deterioration with or without hemorrhage.
- Record: found
- Abstract: not found
- Article: not found