- Record: found
- Abstract: found
- Article: found
Recombinant Human Thyrotropin-Aided Radioiodine Therapy in Patients with Metastatic Differentiated Thyroid Carcinoma
Read this article at
Abstract
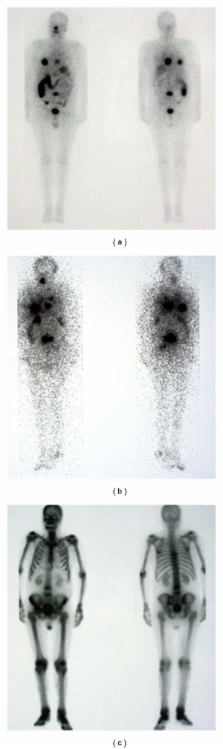
Our aim was to test the efficacy of 131-I therapy (RIT) using recombinant human TSH (rhTSH) in patients with differentiated thyroid carcinoma (DTC) in whom endogenous TSH stimulation was not an option due to the poor patient's physical condition or due to the disease progression during L-thyroxin withdrawal. The study comprised 18 patients, who already have undergone total or near-total thyroidectomy and radioiodine ablation and 0–12 (median 5) RITs after L-thyroxin withdrawal. Our patients received altogether 44 RITs using rhTSH while on L-thyroxin. Six to 12 months after the first rhTSH-aided RIT, PR and SD was achieved in 3/18 (17%) and 4/18 patients (22%), respectively. In most patients ( n = 12; 61%) disease progressed despite rhTSH-aided RITs. As a conclusion, rhTSH-aided RIT proved to add some therapeutic benefit in 39% our patients with metastatic DTC, who otherwise could not be efficiently treated with RIT.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
A comparison of recombinant human thyrotropin and thyroid hormone withdrawal for the detection of thyroid remnant or cancer.
- Record: found
- Abstract: found
- Article: not found
Thyroid hormone withdrawal in patients with differentiated thyroid carcinoma: a one hundred thirty-patient pilot survey on consequences of hypothyroidism and a pharmacoeconomic comparison to recombinant thyrotropin administration.
- Record: found
- Abstract: found
- Article: not found