- Record: found
- Abstract: found
- Article: found
Robotic assisted nephrectomy for living kidney donation (RANLD) with use of multiple locking clips or ligatures for renal vascular closure
Read this article at
Abstract
Background
Robotic assisted nephrectomy for living donation (RANLD) is a rapid emerging surgical technique competing for supremacy with totally laparoscopic and laparoscopic hand assisted techniques. Opinions about the safety of specific techniques of vascular closure in minimally invasive living kidney donation are heterogeneous and may be different for laparoscopic and robotic assisted surgical techniques.
Methods
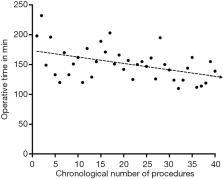
We retrospectively analyzed perioperative and short-term outcomes of our first (n=40) RANLD performed with the da Vinci Si surgical platform. Vascular closure of renal vessels was performed by either double clipping or a combination of clips and non-transfixing suture ligatures.
Results
RANLD almost quintupled in our center for the observed time period. A total of n=21 (52.5%) left and n=19 (47.5%) right kidneys were procured. Renal vessel sealing with two locking clips was performed in 18 cases (45%) Both, clips and non-transfixing ligatures were used in 22 cases (55%). Mean donor age was 53.075±11.68 years (range, 28–70). The average total operative time was 150.75±27.30 min. Right donor nephrectomy (139±22 min) was performed significantly faster than left (160.95±27.93 min, P=0.01). Warm ischemia time was similar for both vascular sealing techniques and did not differ between left and right nephrectomies. No conversion was necessary. Clavien-Dindo Grade ≤IIIb complications occurred in (n=5) 12.5%. Grade IV and V complications did not develop. In particular no hemorrhage occurred using multiple locking clips or suture ligatures for renal vascular closure. Mortality was 0%. Thirteen kidneys (32.5%) were transplanted across the AB0 barrier.
Related collections
Most cited references46

- Record: found
- Abstract: found
- Article: found
KDIGO Clinical Practice Guideline on the Evaluation and Care of Living Kidney Donors
- Record: found
- Abstract: found
- Article: not found
Solid organ transplantation in the 21st century
- Record: found
- Abstract: found
- Article: not found