- Record: found
- Abstract: found
- Article: found
Suicide in England in the COVID-19 pandemic: Early observational data from real time surveillance
Read this article at
Abstract
Background
There have been concerns that the COVID-19 pandemic may lead to an increase in suicide. The coronial system in England is not suitable for timely monitoring of suicide because of the delay of several months before inquests are held.
Methods
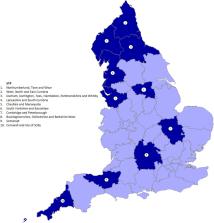
We used data from established systems of "real time surveillance" (RTS) of suspected suicides, in areas covering a total population of around 13 million, to test the hypothesis that the suicide rate rose after the first national lockdown began in England.
Findings
The number of suicides in April-October 2020, after the first lockdown began, was 121•3 per month, compared to 125•7 per month in January-March 2020 (-4%; 95% CI-19% to 13%, p = 0•59). Incidence rate ratios did not show a significant rise in individual months after lockdown began and were not raised during the 2-month lockdown period April-May 2020 (IRR: 1•01 [0•81–1•25]) or the 5-month period after the easing of lockdown, June-October 2020 (0•94 [0•81–1•09]). Comparison of the suicide rates after lockdown began in 2020 for the same months in selected areas in 2019 showed no difference.
Interpretation
We did not find a rise in suicide rates in England in the months after the first national lockdown began in 2020, despite evidence of greater distress. However, a number of caveats apply. These are early figures and may change. Any effect of the pandemic may vary by population group or geographical area. The use of RTS in this way is new and further development is needed before it can provide full national data.
Funding
This study was funded by the Healthcare Quality Improvement Partnership (HQIP).The HQIP is led by a consortium of the Academy of Medical Royal Colleges, the Royal College of Nursing, and National Voices. Its aim is to promote quality improvement in patient outcomes, and in particular, to increase the impact that clinical audit, outcome review programs and registries have on healthcare quality in England and Wales. HQIP holds the contract to commission, manage, and develop the National Clinical Audit and Patient Outcomes Program (NCAPOP), comprising around 40 projects covering care provided to people with a wide range of medical, surgical and mental health conditions. The program is funded by NHS England, the Welsh Government and, with some individual projects, other devolved administrations, and crown dependencies.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: found
Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science
- Record: found
- Abstract: found
- Article: not found
Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population

- Record: found
- Abstract: found
- Article: found