- Record: found
- Abstract: found
- Article: found
IMI – Myopia Control Reports Overview and Introduction
Read this article at
Abstract
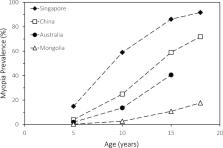
With the growing prevalence of myopia, already at epidemic levels in some countries, there is an urgent need for new management approaches. However, with the increasing number of research publications on the topic of myopia control, there is also a clear necessity for agreement and guidance on key issues, including on how myopia should be defined and how interventions, validated by well-conducted clinical trials, should be appropriately and ethically applied. The International Myopia Institute (IMI) reports the critical review and synthesis of the research evidence to date, from animal models, genetics, clinical studies, and randomized controlled trials, by more than 85 multidisciplinary experts in the field, as the basis for the recommendations contained therein. As background to the need for myopia control, the risk factors for myopia onset and progression are reviewed. The seven generated reports are summarized: (1) Defining and Classifying Myopia, (2) Experimental Models of Emmetropization and Myopia, (3) Myopia Genetics, (4) Interventions for Myopia Onset and Progression, (5) Clinical Myopia Control Trials and Instrumentation, (6) Industry Guidelines and Ethical Considerations for Myopia Control, and (7) Clinical Myopia Management Guidelines.
Related collections
Most cited references116
- Record: found
- Abstract: found
- Article: found
Systems for grading the quality of evidence and the strength of recommendations I: Critical appraisal of existing approaches The GRADE Working Group

- Record: found
- Abstract: found
- Article: found
IMI – Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies
- Record: found
- Abstract: found
- Article: not found