- Record: found
- Abstract: found
- Article: found
Quantification of Treatment Effect Modification on Both an Additive and Multiplicative Scale
Read this article at
Abstract
Background
In both observational and randomized studies, associations with overall survival are by and large assessed on a multiplicative scale using the Cox model. However, clinicians and clinical researchers have an ardent interest in assessing absolute benefit associated with treatments. In older patients, some studies have reported lower relative treatment effect, which might translate into similar or even greater absolute treatment effect given their high baseline hazard for clinical events.
Methods
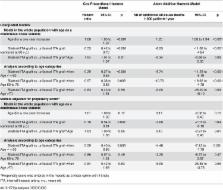
The effect of treatment and the effect modification of treatment were respectively assessed using a multiplicative and an additive hazard model in an analysis adjusted for propensity score in the context of coronary surgery.
Results
The multiplicative model yielded a lower relative hazard reduction with bilateral internal thoracic artery grafting in older patients (Hazard ratio for interaction/year = 1.03, 95%CI: 1.00 to 1.06, p = 0.05) whereas the additive model reported a similar absolute hazard reduction with increasing age (Delta for interaction/year = 0.10, 95%CI: -0.27 to 0.46, p = 0.61). The number needed to treat derived from the propensity score-adjusted multiplicative model was remarkably similar at the end of the follow-up in patients aged < = 60 and in patients >70.
Conclusions
The present example demonstrates that a lower treatment effect in older patients on a relative scale can conversely translate into a similar treatment effect on an additive scale due to large baseline hazard differences. Importantly, absolute risk reduction, either crude or adjusted, can be calculated from multiplicative survival models. We advocate for a wider use of the absolute scale, especially using additive hazard models, to assess treatment effect and treatment effect modification.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Estimating measures of interaction on an additive scale for preventive exposures
- Record: found
- Abstract: found
- Article: not found
