- Record: found
- Abstract: found
- Article: found
One Health in hospitals: how understanding the dynamics of people, animals, and the hospital built-environment can be used to better inform interventions for antimicrobial-resistant gram-positive infections
Read this article at
Abstract
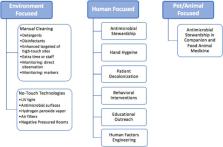
Despite improvements in hospital infection prevention and control, healthcare associated infections (HAIs) remain a challenge with significant patient morbidity, mortality, and cost for the healthcare system. In this review, we use a One Health framework (human, animal, and environmental health) to explain the epidemiology, demonstrate key knowledge gaps in infection prevention policy, and explore improvements to control Gram-positive pathogens in the healthcare environment. We discuss patient and healthcare worker interactions with the hospital environment that can lead to transmission of the most common Gram-positive hospital pathogens – methicillin-resistant Staphylococcus aureus, Clostridioides ( Clostridium) difficile, and vancomycin-resistant Enterococcus – and detail interventions that target these two One Health domains. We discuss the role of animals in the healthcare settings, knowledge gaps regarding their role in pathogen transmission, and the absence of infection risk mitigation strategies targeting animals. We advocate for novel infection prevention and control programs, founded on the pillars of One Health, to reduce Gram-positive hospital-associated pathogen transmission.
Related collections
Most cited references131
- Record: found
- Abstract: found
- Article: not found
Invasive methicillin-resistant Staphylococcus aureus infections in the United States.
- Record: found
- Abstract: found
- Article: not found
Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic.
- Record: found
- Abstract: found
- Article: not found