INTRODUCTION
Mitral regurgitation in dilated cardiomyopathy is often a functional reason of either ischemic or idiopathic origin. Persistent severe mitral regurgitation leads to left ventricular and atrial chamber remodeling with poor clinical outcomes [1]. In most patients, effective surgical repair of the mitral valve causes a decrease in the left ventricular volume overload and leads to reverse left ventricular and left atrial remodeling [2]. In cases of patients with high comorbidity and higher mortality after surgery, less invasive catheter-based techniques have been developed. The MONARC device (Edwards Livesciences) is implanted in the coronary sinus as an indirect annuloplasty. It is constructed of nitinol and consists of a larger proximal anchor, a bridge segment with bio-absorbing coating, and a smaller distal anchor. In the Evolution I study, a patient with functional mitral regurgitation between 2+ and 4+ revealed at 12 months a reduction by >1 grade in 50%, that is less than what it obtained with surgical mitral valve repair. Patients with severe mitral regurgitation (grade >3+) seemed most likely benefitted [3]. Mitral valve repair is performed to reduce the mitral regurgitation by creating a double orifice that was first performed by Alfiri [4]. Based on this surgical technique, endovascular mitral repair has been developed with the use of a clip [5]. The posterior and the anterior leaflets are joined by implanting one or more clips resulting in reduction of mitral regurgitation. Percutaneous mitral valve repair in edge-to-edge procedure with the MitalClip device has been shown to be associated with good clinical outcomes in patients with high risk for surgery [6]. Furthermore, it demonstrated superior safety compared to surgical mitral valve repair with similar improvement in clinical outcomes [7]. In contrast to the MONARC device, the MitraClip can be used for both functional and structural mitral regurgitations.
CASE REPORT
We describe a case of a 73-year-old man with severe mitral regurgitation in ischemic cardiomyopathy and implanted MONARC device four years ago. The medical history included an ischemic cardiomyopathy with highly reduced ejection fraction (30%). He had a single bypass surgery in 1995 (RIVA) and stenting of the RCX in 2009. A defibrillator was implanted in case of ventricular tachycardia. Furthermore, he had impaired renal function and a moderately combined lung disease (Euroscore 51%). In 2009, he was included in the Evolutian trial and got uncomplicated a 120 cm 6/15 mm anchor (Figure 1) with a reduction of the mitral regurgitation from grade 3 to 2 after six months. Since the end of 2010, a continuing increase in mitral regurgitation was documented with a parallel increase in the New York Heart Association (NYHA) class. In the beginning of 2013 he had dyspnoea with minimal exercise and a documented high grade mitral regurgitation. So we decided on the implantation of a MitraClip.
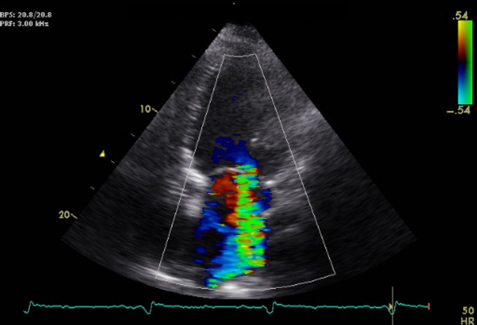
The pre-procedural echocardiogram revealed a dilated left ventricle with end-diastolic dimension of 71 mm and serve reduced left ventricular function with 35%. We had a bi-atrial dilatation with 213 ml for the left atrium and 112 ml for the right atrium with severe mitral regurgitation and minimal tricuspid regurgitation (Figure 2). The right ventricular systolic pressure was 45 mmHg, confirming pulmonary hypertension. The trans-esophageal echocardiogram conformed severe mitral regurgitation (Figure 3). With a three-dimensional echocardiogram, we evaluated the possibility of MitraClip by enough leaflet substance without presentation of serve prolapse or structural disintegrity. Through the implanted MONARC device, a bowing posterior annulus was documented and it was difficult to evaluate the posterior leaflet length and integrity (Figure 4).

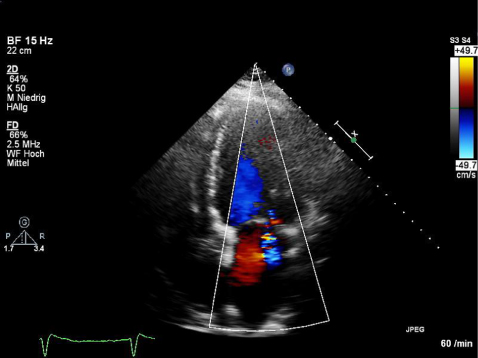
The standard procedure was performed with percutaneous femoral venous transseptal access. The clip was aligned above the mitral valve, approved with a three-dimensional echocardiogram, before grasping and coapting the leaflets. The grasp of the leaflets was difficult in case of the bowing posterior annulus and shadow of the MONARC device. After the first grasping and clip placement, we demonstrated a reduction of the mitral regurgitation from grade 3 to 1–2 with a remaining jet lateral of the clip. The verification of the leaflet insertion confirmed enough stuff of the posterior leaflet as well as of the anterior leaflet in the clip. With the second clip, we could reduce the mitral regurgitation to grade 0–1 (Figure 5, Supplementary Video 1).
The procedure was completed and the anesthesia was stopped. The patient was awake and hemodynamically steady. The post-interventional echocardiogram on day 3 confirmed minimal residual regurgitation without stenosis and a re-gradient right ventricular systolic pressure to 32 mmHg by constant minimal tricuspid regurgitation.
DISCUSSION
The MONARC device implantation showed a response of 50% with the reduction in mitral regurgitation of grade 1 after 6–12 months, and the patients with severe initial mitral regurgitation seemed most likely benefitted. Furthermore, only the functional regurgitation is influenced. Mitral clipping is an attractive alternative treatment of severe mitral regurgitation, and, in contrast, it can be used for functional and structural mitral valve regurgitations. In addition, we have a direct effect of reduction after clipping, and the clinical improvement is instant.