- Record: found
- Abstract: found
- Article: found
Outcome and Toxicity Patterns in Children and Adolescents with Non-Hodgkin Lymphoma: A Single Institution Experience
Read this article at
Abstract
Background
The incidence and biology of non-Hodgkin lymphoma (NHL) vary according to age. Some data suggest that the impact of age in pediatric and adolescent NHL patients depends on the histological subtype. Objectives: We aimed to analyze the impact of age at diagnosis on clinical characteristics and treatment-related toxicity in children and adolescents with NHL.
Methods
Retrospective review of medical records of children and adolescents diagnosed with NHL at the Hospital for Sick Children, Toronto, between January 1995 and December 2008.
Results
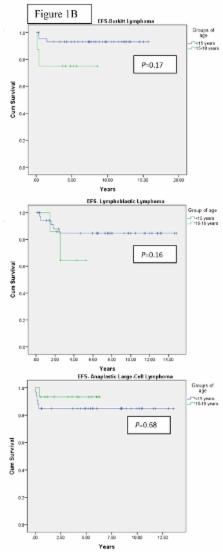
164 children were diagnosed with NHL during the study period, with a median age at diagnosis of 10 years. With a median follow-up of 6.2 years, 5-year OS in patients aged <15 and 15–18 years was 89± 2% vs 82% ± 6%, respectively ( P = 0.30), and 5-year EFS was 84% ± 3% vs. 77% ± 7% ( P= 0.37). In Burkitt’s lymphoma (BL) and lymphoblastic lymphoma (LL) there was a trend towards better outcomes in children compared to adolescents, with EFS of 91% ± 4% vs. 75% ± 15%, respectively in BL ( P= 0.17), and 82% ± 7% vs. 51.4% ± 2% respectively in LL ( P= 0.16). Late effects occurred in 21 patients (12.8%).
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: not found
CD30(+) anaplastic large cell lymphoma: a review of its histopathologic, genetic, and clinical features.
- Record: found
- Abstract: found
- Article: not found
The Société Française d'Oncologie Pédiatrique LMB89 protocol: highly effective multiagent chemotherapy tailored to the tumor burden and initial response in 561 unselected children with B-cell lymphomas and L3 leukemia.
- Record: found
- Abstract: found
- Article: not found