- Record: found
- Abstract: found
- Article: found
Obstetric Volume and Severe Maternal Morbidity Among Low-Risk and Higher-Risk Patients Giving Birth at Rural and Urban US Hospitals

Read this article at
Abstract
This cross-sectional study assesses associations between obstetric volume and severe maternal morbidity in rural and urban hospitals and examines whether these associations differ for low-risk and higher-risk patients.
Key Points
Question
What is the association between obstetric volume and severe maternal morbidity in US rural and urban hospitals, and do these associations differ for low-risk and higher-risk patients?
Findings
In this cross-sectional study of more than 11 million births in urban counties and 519 953 births in rural counties, risk of severe maternal morbidity was elevated for low-risk and higher-risk obstetric patients who gave birth in lower-volume rural hospitals, compared with similar patients who gave birth at rural hospitals with more than 460 annual births. No significant volume-outcome association was detected among urban hospitals.
Abstract
Importance
Identifying hospital factors associated with severe maternal morbidity (SMM) is essential to clinical and policy efforts.
Objective
To assess associations between obstetric volume and SMM in rural and urban hospitals and examine whether these associations differ for low-risk and higher-risk patients.
Design, Setting, and Participants
This retrospective cross-sectional study of linked vital statistics and patient discharge data was conducted from 2022 to 2023. Live births and stillbirths (≥20 weeks’ gestation) at hospitals in California (2004-2018), Michigan (2004-2020), Pennsylvania (2004-2014), and South Carolina (2004-2020) were included. Data were analyzed from December 2022 to May 2023.
Exposures
Annual birth volume categories (low, medium, medium-high, and high) for hospitals in urban (10-500, 501-1000, 1001-2000, and >2000) and rural (10-110, 111-240, 241-460, and >460) counties.
Main Outcome and Measures
The main outcome was SMM (excluding blood transfusion); covariates included age, payer status, educational attainment, race and ethnicity, and obstetric comorbidities. Analyses were stratified for low-risk and higher-risk obstetric patients based on presence of at least 1 clinical comorbidity.
Results
Among more than 11 million urban births and 519 953 rural births, rates of SMM ranged from 0.73% to 0.50% across urban hospital volume categories (high to low) and from 0.47% to 0.70% across rural hospital volume categories (high to low). Risk of SMM was elevated for patients who gave birth at rural hospitals with annual birth volume of 10 to 110 (adjusted risk ratio [ARR], 1.65; 95% CI, 1.14-2.39), 111 to 240 (ARR, 1.37; 95% CI, 1.10-1.70), and 241 to 460 (ARR, 1.26; 95% CI, 1.05-1.51), compared with rural hospitals with greater than 460 births. Increased risk of SMM occurred for low-risk and higher-risk obstetric patients who delivered at rural hospitals with lower birth volumes, with low-risk rural patients having notable discrepancies in SMM risk between low (ARR, 2.32; 95% CI, 1.32-4.07), medium (ARR, 1.66; 95% CI, 1.20-2.28), and medium-high (ARR, 1.68; 95% CI, 1.29-2.18) volume hospitals compared with high volume (>460 births) rural hospitals. Among hospitals in urban counties, there was no significant association between birth volume and SMM for low-risk or higher-risk obstetric patients.
Conclusions and Relevance
In this cross-sectional study of births in US rural and urban counties, risk of SMM was elevated for low-risk and higher-risk obstetric patients who gave birth in lower-volume hospitals in rural counties, compared with similar patients who gave birth at rural hospitals with greater than 460 annual births. These findings imply a need for tailored quality improvement strategies for lower volume hospitals in rural communities.
Related collections
Most cited references34
- Record: found
- Abstract: found
- Article: found
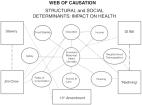
Social and Structural Determinants of Health Inequities in Maternal Health
- Record: found
- Abstract: not found
- Article: not found
Severe Maternal Morbidity Among Delivery and Postpartum Hospitalizations in the United States
- Record: found
- Abstract: found
- Article: not found