- Record: found
- Abstract: found
- Article: found
Which score should be used in intubated patients’ Glasgow coma scale or full outline of unresponsiveness?
Read this article at
Abstract
Background and Aims:
Today Glasgow coma scale (GCS) is the most well-known and common score for evaluation of the level of consciousness and outcome predict after traumatic brain injuries in the world. Regarding to some advantages of the full outline of unresponsiveness (FOUR) score over GCS in intubated patients, we’re going to compare the precision of these two scores in predicting the outcome predict in intubated patients.
Methods:
This research was a diagnostic-based study, which was conducted prospectively on 80 patients with Traumatic brain injury who were intubated and admitted to Intensive Care Unit (ICU) of Educational Hospitals of Mazandaran University of Medical Science during February 2013 to August 2013. The scores of FOUR and GCS were measured by the researcher in the first 24 h of admission in ICU. The information's recorded in the check list including the mortality rate of early and late inside of the hospital interred to excel. The findings were analyzed using SPSS software, through descriptive statistics and regression logistic.
Results:
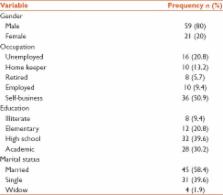
The results showed of 80 patients 21 patients (20%) were female and 59 patients (80%) were male. The age average of the samples was 33.80 ± 12.60 ranging from 16 to 60 years old. 21 patients (26.2%) died during treatment. Of 21 patients, 15 patients died during first 14 days (18.7%) and 6 patients died after 14 years (7.5%). The area under curve (AUC) of FOUR score in early mortality was 0.90 (C 1 = 0.95, 0.88–0.90). The amount AUC for GCS was 0.80 (C 1 = 0.95, 0.78–0.84), which in delayed mortality it was ordered as 0.86 (C 1 = 0.95, 0.84–0.90) and 0.89 (C 1 = 0.95, 0.78–0.88).
Conclusion:
The research results indicated that FOUR score is more exact and more practical in intubated patients regarding lack of verbal response factor in early mortality prediction in GCS. Hence, it is recommended for health professionals to use the FOUR score to predict the early outcome of intubated patients with traumatic brain injuries.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Variations in mortality and length of stay in intensive care units.
- Record: found
- Abstract: found
- Article: not found