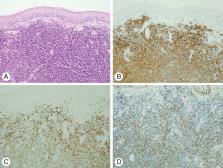
Mantle cell lymphoma (MCL) is a non-Hodgkin lymphoma characterized by involvement of the lymph nodes, spleen, blood, and bone marrow with a short remission duration to standard therapies and a median overall survival of 4-5 years. Diagnosis is based on lymph node, bone marrow, or tissue morphology of centrocytic lymphocytes, small cell type, or blastoid variant cells. A chromosomal translocation t(11:14) is the molecular hallmark of MCL, resulting in the overexpression of cyclin D1. Cyclin D1 is detected by immunohistochemistry in 98% of cases. The absence of SOX-11 or a low Ki-67 may correlate with a more indolent form of MCL. The differential diagnosis of MCL includes small lymphocytic lymphoma, marginal zone lymphoma, and follicular lymphoma. The mantle cell lymphoma international prognostic index (MIPI) is the prognostic model most often used and incorporates ECOG performance status, age, leukocyte count, and lactic dehydrogenase. A modification of the MIPI also adds the Ki-67 proliferative index if available. The median overall survival (OS) for the low-risk group was not reached (5-year OS of 60%). The median OS for the intermediate risk group was 51 and 29 months for the high-risk group. For selected indolent, low MIPI MCL patients, initial observation may be appropriate therapy. For younger patients with intermediate or high risk MIPI MCL, aggressive therapy with a cytarabine containing regimen ± autologous stem cell transplantation should be considered. For older MCL patients with intermediate or high risk MIPI, combination chemotherapy with R-CHOP, R-Bendamustine, or a clinical trial should be considered. At the time of relapse, agents directed at activated pathways in MCL cells such as bortezomib (NFkB inhibitor), BTK inhibitors or CAL-101 (B-cell receptor inhibitors) or lenalidamide (antiangiogenesis) have clinical activity in MCL patients. Autologous or allogeneic stem cell transplantation can also be considered in young patients. Copyright © 2012 Wiley Periodicals, Inc.