- Record: found
- Abstract: found
- Article: found
Protective Behaviors and Secondary Harms Resulting From Nonpharmaceutical Interventions During the COVID-19 Epidemic in South Africa: Multisite, Prospective Longitudinal Study
Abstract
Background
In March 2020, South Africa implemented strict nonpharmaceutical interventions (NPIs) to contain the spread of COVID-19. Over the subsequent 5 months, NPI policies were eased in stages according to a national strategy. COVID-19 spread throughout the country heterogeneously; the disease reached rural areas by July and case numbers peaked from July to August. A second COVID-19 wave began in late 2020. Data on the impact of NPI policies on social and economic well-being and access to health care are limited.
Objective
We aimed to determine how rural residents in three South African provinces changed their behaviors during the first COVID-19 epidemic wave.
Methods
The South African Population Research Infrastructure Network nodes in the Mpumalanga (Agincourt), KwaZulu-Natal, (Africa Health Research Institute) and Limpopo (Dikgale-Mamabolo-Mothiba) provinces conducted up to 14 rounds of longitudinal telephone surveys among randomly sampled households from rural and periurban surveillance populations every 2-3 weeks. Interviews included questions on the following topics: COVID-19–related knowledge and behaviors, the health and economic impacts of NPIs, and mental health. We analyzed how responses varied based on NPI stringency and household sociodemographics.
Results
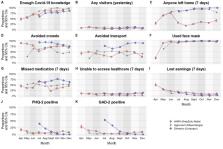
In total, 5120 households completed 23,095 interviews between April and December 2020. Respondents’ self-reported satisfaction with their COVID-19–related knowledge and face mask use rapidly rose to 85% and 95%, respectively, by August. As selected NPIs were eased, the amount of travel increased, economic losses were reduced, and the prevalence of anxiety and depression symptoms fell. When the number of COVID-19 cases spiked at one node in July, the amount of travel dropped rapidly and the rate of missed daily medications doubled. Households where more adults received government-funded old-age pensions reported concerns about economic matters and medication access less often.
Conclusions
South Africans complied with stringent, COVID-19–related NPIs despite the threat of substantial social, economic, and health repercussions. Government-supported social welfare programs appeared to buffer interruptions in income and health care access during local outbreaks. Epidemic control policies must be balanced against the broader well-being of people in resource-limited settings and designed with parallel support systems when such policies threaten peoples’ income and access to basic services.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
An interactive web-based dashboard to track COVID-19 in real time
- Record: found
- Abstract: found
- Article: not found
Impact of COVID-19 Pandemic on Mental Health in the General Population: A Systematic Review
- Record: found
- Abstract: found
- Article: not found