- Record: found
- Abstract: found
- Article: found
Using Period Analysis to Timely Assess and Predict 5-Year Relative Survival for Liver Cancer Patients From Taizhou, Eastern China
Read this article at
Abstract
Introduction
While timely assessment of long-term survival for patients with liver cancer is essential for the evaluation of early detection and screening programs of liver cancer, those data are extremely scarce in China. We aimed to timely and accurately assess long-term survival for liver cancer patients in eastern China.
Methods
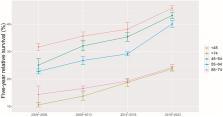
Patients diagnosed with liver cancer during 2004–2018 from four cancer registries with high-quality data from Taizhou, eastern China, were included. The period analysis was used to calculate the 5-year relative survival (RS) for overall and the stratification by sex, age at diagnosis, and region. The projected 5-year RS of liver cancer patients during 2019–2023 was also assessed using a model-based period analysis.
Results
The overall 5-year RS for patients with liver cancer during 2014–2018 reached 32.4%, being 29.3% for men and 36.1% for women. The 5-year RS declined along with aging, decreasing from 38.2% for age <45 years to 18.8% for age >74 years, while the 5-year RS for urban area was higher compared to rural area (36.8% vs. 29.3%). The projected overall 5-year RS of liver cancer patients could reach 41.4% during the upcoming period 2019–2023.
Conclusions
We provided, for first time in China using the period analysis, the most up-to-date 5-year RS for patients with liver cancer from Taizhou, eastern China, and also found that the 5-year RS for liver cancer patients have improved greatly during 2004–2018, which has important implications for the timely evaluation of early detection and screening programs for patients with liver cancer in eastern China.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries
- Record: found
- Abstract: found
- Article: not found
