- Record: found
- Abstract: found
- Article: found
Multimorbidity patterns in the elderly: a prospective cohort study with cluster analysis
Read this article at
Abstract
Background
Multimorbidity is the coexistence of more than two chronic diseases in the same individual; however, there is no consensus about the best definition. In addition, few studies have described the variability of multimorbidity patterns over time. The aim of this study was to identify multimorbidity patterns and their variability over a 6-year period in patients older than 65 years attended in primary health care.
Methods
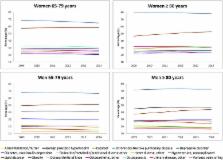
A cohort study with yearly cross-sectional analysis of electronic health records from 50 primary health care centres in Barcelona. Selected patients had multimorbidity and were 65 years of age or older in 2009. Diagnoses (International Classification of Primary Care, second edition) were extracted using O’Halloran criteria for chronic diseases. Multimorbidity patterns were identified using two steps: 1) multiple correspondence analysis and 2) k-means clustering. Analysis was stratified by sex and age group (65–79 and ≥80 years) at the beginning of the study period.
Results
Analysis of 2009 electronic health records from 190,108 patients with multimorbidity (59.8% women) found a mean age of 71.8 for the 65–79 age group and 84.16 years for those over 80 (Standard Deviation [SD] 4.35 and 3.46, respectively); the median number of chronic diseases was seven (Interquartil range [IQR] 5–10). We obtained 6 clusters of multimorbidity patterns (1 nonspecific and 5 specifics) in each group, being the specific ones: Musculoskeletal, Endocrine-metabolic, Digestive/Digestive-respiratory, Neurological, and Cardiovascular patterns. A minimum of 42.5% of the sample remained in the same pattern at the end of the study, reflecting the stability of these patterns.
Conclusions
This study identified six multimorbidity patterns per each group, one nonnspecific pattern and five of them with a specific pattern related to an organic system. The multimorbidity patterns obtained had similar characteristics throughout the study period. These data are useful to improve clinical management of each specific subgroup of patients showing a particular multimorbidity pattern.
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study.
- Record: found
- Abstract: found
- Article: not found
Aging with multimorbidity: a systematic review of the literature.

- Record: found
- Abstract: found
- Article: found